COVID-19 SEROPREVALENCE AMONG ROYAL THAI ARMY PERSONNEL IN BANGKOK METROPOLITAN AREA FROM JULY-SEPTEMBER 2020
DOI:
https://doi.org/10.55374/jseamed.v4i2.76Keywords:
COVID-19 infection, Military personnel, Bangkok Metropolitan AreaAbstract
Background: COVID-19 is an ongoing pandemic that causes millions of deaths worldwide. Seroprevalence studies play a crucial role in identifying asymptomatic infection and providing the true prevalence of COVID-19 in the community. However, no COVID-19 seroprevalence in Thailand has been reported before.
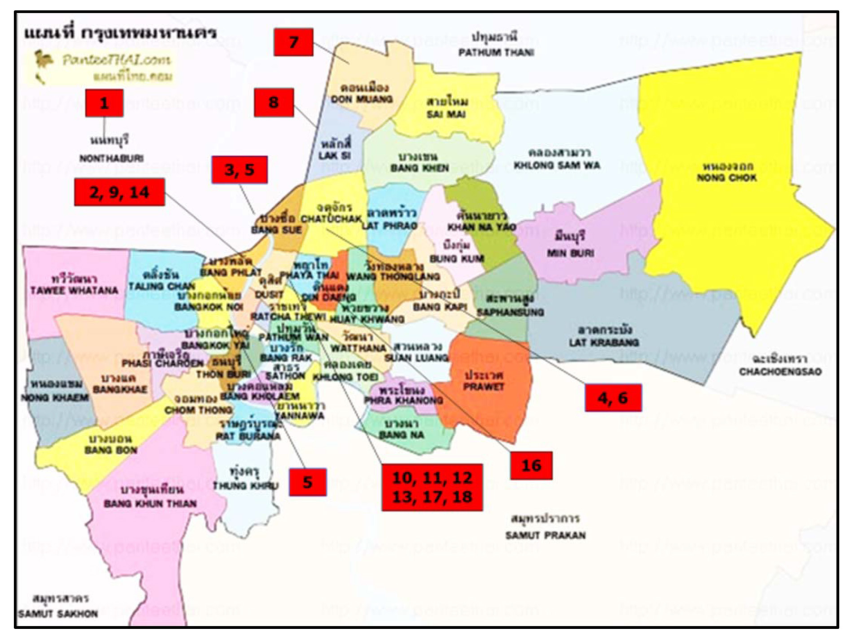
Objective: The study aimed to measure the prevalence of the SARS-CoV-2 antibody among army personnel residing in the Bangkok Metropolitan Area.
Methods: All army personnel receiving health checkups from 1 July - 30 September 2020 were invited to participate in the study after providing informed consent. The seroprevalence was conducted using leftover serum without additional venipuncture. The screening conducted using the Rapid test by Wondfo®. When a screening test was positive, a confirmation test would be performed using ELISA by EuroImmun®. In case of a positive ELISA confirmation test result, the COVID-19 investigation team would be activated and deployed.
Results: In all, 6,651 army personnel participated in this study. The age of participants ranged from 20-60 years with mean age of 40.5+12.02. Most participants were male (85.5%). The rapid screening test using Wondfo® was positive in 41 cases (0.61%). The confirmation test using ELISA yielded a positive result in 1 subject (0.015%). That person was a known case of COVID-19 infection, who received a full course of treatment and was confirmed to have negative RT-PCR before being discharged from the hospital a few weeks earlier.
Conclusion: This was the first large scale seroprevalence surveillance of COVID-19 in Thailand. Our study revealed no new detectable case of asymptomatic COVID-19 infection in the Bangkok Metropolitan Area.
Downloads
Metrics
References
Czernin J. Dr. Li Wenliang and the Time of COVID-19. J Nucl Med 2020; 61: 625. DOI: https://doi.org/10.2967/jnumed.120.245712
Li X, Cui W, Zhang F. Who Was the First Doctor to Report the COVID-19 Outbreak in Wuhan, China? J Nucl Med 2020; 61: 782-3. DOI: https://doi.org/10.2967/jnumed.120.247262
Bernard Stoecklin S, Rolland P, Silue Y, Mailles A, Campese C, Simondon A, et al. First cases of coronavirus disease 2019 (COVID-19) in France: surveillance, investigations and control measures, January 2020. Euro Surveill 2020;25(6). DOI: https://doi.org/10.2807/1560-7917.ES.2020.25.6.2000094
Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med 2020; 382: 929-36. DOI: https://doi.org/10.1056/NEJMoa2001191
Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet 2020; 395: 1225-8. DOI: https://doi.org/10.1016/S0140-6736(20)30627-9
Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med 2020; 382: 1199-207. DOI: https://doi.org/10.1056/NEJMoa2001316
Okada P, Buathong R, Phuygun S, Thanadachakul T, Parnmen S, Wongboot W, et al. Early transmission patterns of coronavirus disease 2019 (COVID-19) in travellers from Wuhan to Thailand, January 2020. Euro Surveill 2020; 25(8). DOI: https://doi.org/10.2807/1560-7917.ES.2020.25.8.2000097
Ng DL, Goldgof GM, Shy BR, Levine AG, Balcerek J, Bapat SP, et al. SARS-CoV-2 seroprevalence and neutralizing activity in donor and patient blood. Nat Commun 2020; 11: 4698 DOI: https://doi.org/10.1038/s41467-020-18468-8
Pollan M, Perez-Gomez B, Pastor-Barriuso R, Oteo J, Hernan MA, Perez-Olmeda M, et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, populationbased seroepidemiological study. Lancet 2020; 396: 535-44. DOI: https://doi.org/10.1016/S0140-6736(20)31483-5
Sood N, Simon P, Ebner P, Eichner D, Reynolds J, Bendavid E, et al. Seroprevalence of SARS-CoV-2-Specific Antibodies Among Adults in Los Angeles County, California, on April 10-11, 2020. JAMA 2020; 323: 2425-7. DOI: https://doi.org/10.1001/jama.2020.8279
Stringhini S, Wisniak A, Piumatti G, Azman AS, Lauer SA, Baysson H, et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study. Lancet 2020; 396: 313-9. DOI: https://doi.org/10.1016/S0140-6736(20)31304-0
Xu X, Sun J, Nie S, Li H, Kong Y, Liang M, et al. Author Correction: Seroprevalence of immunoglobulin M and G antibodies against SARS-CoV-2 in China. Nat Med 2020; 26: 1494. DOI: https://doi.org/10.1038/s41591-020-1058-2
2020 [Available from: https://www.bilcare.com/SARS-CoV-2%20Antibody%20Test%20(Lateral%20Flow%20Method).pdf
Wu JL, Tseng WP, Lin CH, Lee TF, Chung MY, Huang CH, et al. Four point-of-care lateral flow immunoassays for diagnosis of COVID-19 and for assessing dynamics of antibody responses to SARS-CoV-2. J Infect 2020; 81: 435-42. DOI: https://doi.org/10.1016/j.jinf.2020.06.023
Serrano MM, Rodriguez DN, Palop NT, Arenas RO, Cordoba MM, Mochon MDO, et al. Comparison of commercial lateral flow immunoassays and ELISA for SARS-CoV-2 antibody detection. J Clin Virol 2020; 129: 104529. DOI: https://doi.org/10.1016/j.jcv.2020.104529
Santos VAD, Rafael MM, Sabino EC, Duarte A. Sensitivity of the Wondfo One Step COVID-19 test using serum samples. Clinics (Sao Paulo) 2020; 75: e2013. DOI: https://doi.org/10.6061/clinics/2020/e2013
Charlton CL, Kanji JN, Johal K, Bailey A, Plitt SS, MacDonald C, et al. Evaluation of Six Commercial Mid- to High-Volume Antibody and Six Point-of-Care Lateral Flow Assays for Detection of SARS-CoV-2 Antibodies. J Clin Microbiol 2020; 58: e01361-20. DOI: https://doi.org/10.1128/JCM.01361-20
Hilborne LH, Wagner Z, Cabreros I, Brook RH. Linking Statistics With Testing Policy to Manage COVID-19 in the Community. Am J Clin Pathol 2020; 154: 142-8. DOI: https://doi.org/10.1093/ajcp/aqaa099
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.