COMPARISON BETWEEN IMAGE-FREE ROBOTIC ASSISTED AND CONVENTIONAL TOTAL KNEE ARTHROPLASTY: POSTOPERATIVE CT ASSESSMENT OF ALIGNMENT
DOI:
https://doi.org/10.55374/jseamed.v4i1.69Keywords:
Image-free robotic assisted TKA, Robotic knee surgery, Rotational axis alignment, NAVIO, Mechanical axis alignmentAbstract
Background: Navio Surgical System, a newer-generation robotic technology, is an image-free roboticassisted total knee arthroplasty (TKA) offering several advantages over older versions, including CT scan, the potential to dynamically assess soft tissue over a range of motion and the ability to use haptic control in bone preparation.
Objective: The study aimed to compare the accuracy of component alignment between image-free robotic-assisted and conventional TKA.
Methods: Forty patients were randomly assigned to two groups, 20 image-free robotic-assisted and 20 conventional TKA. The primary outcome was prosthetic alignment including mechanical axis alignment, epicondylar axis alignment and posterior tibial slope. The secondary outcomes included postoperative blood loss and operative time.
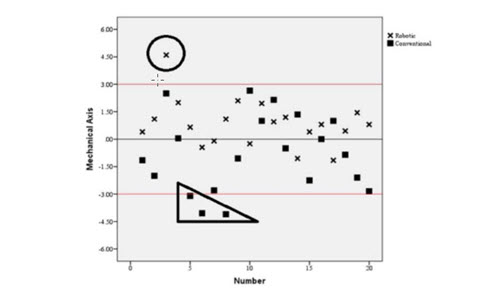
Results: Significant difference were found in the postoperative mechanical axis between the image-free robotic group and the conventional group (1.15°±1° vs. 1.88°±1.19° deviated from neutral mechanical alignment, p = 0.043). There was significant difference in femoral rotational alignment between groups (1.00°±0.75° vs. 2.33°±0.96° deviated from the epicondylar axis, p<0.001). The mean posterior tibial slope did not significantly differ (3.89°±1.66° vs. 4.12°±1.37°, p=0.639). The operative time in the image-free robotic group was significantly longer than that of the conventional group (102.80 ± 11.18 min vs. 62.90 ± 3.28 min, p <0.001). Total blood loss in the image-free robotic group was significantly higher than conventional group (2.24±0.49 g/dl vs. 1.64±0.68 g/dl, p = 0.001).
Conclusion: Image-free robotic-assisted TKA constituted a surgical procedure which could provide better accuracy in prosthetic alignment in both mechanical axis and rotational axis compared with conventional TKA. However, the image-free robotic assisted TKA involved higher blood loss and longer operative time.
Downloads
Metrics
References
Cates HE, Ritter MA, Keating EM, Faris PM. Intra-medullary femoral alignment systems in total knee replacement. Colin Orthop Relat Res 1993; 286: 32-9. DOI: https://doi.org/10.1097/00003086-199301000-00007
Peterson TL, Engh GA. Radiographic assessment of knee alignment after total knee arthroplasty. J Arthroplasty 1988; 3: 67-72. DOI: https://doi.org/10.1016/S0883-5403(88)80054-8
Simmons ED Jr, Sullivan JA, Rackemann S, Scott RD. The accuracy of tibial intramedullary alignment devices in total knee arthroplasty. J Arthroplasty 1991; 6: 45-50. DOI: https://doi.org/10.1016/S0883-5403(06)80156-7
Dennis DA, Channer M, Susan MH, Stringer EA. Intramedullary versus extramedullary tibial alignment systems in total knee arthroplasty. J Arthroplasty 1993; 8: 43-7. DOI: https://doi.org/10.1016/S0883-5403(06)80106-3
Furnes O, Espehaug B, Lie SA, Vollset SE, Engesaeter LB, Havelin LI. Failure mechanisms after unicompartmental and tricompartmental primary knee replacement with cement. J Bone Joint Surg 2007; 89: 519–25. DOI: https://doi.org/10.2106/JBJS.F.00210
Scuderi GR, Insall JN, Windsor RE, Moran MC. Survivorship of cemented knee replacements. J Bone Joint Surg Br 1989; 71: 798–803. DOI: https://doi.org/10.1302/0301-620X.71B5.2584250
Emmerson KP, Moran CG, Pinder IM. Survivorship analysis of the Kinematic Stabilizer total knee replacement: a 10-to 14-year follow-up. J Bone Joint Surg Br 1996; 78-B: 441–5. DOI: https://doi.org/10.1302/0301-620X.78B3.0780441
Ranawat CS, Flynn WF, Saddler S, Hansraj KK, Maynard MJ. Long-term results of the total condylar knee arthroplasty. A 15-year survivorship study. Clin Orthop Relat Res 1993; 286: 94–102. DOI: https://doi.org/10.1097/00003086-199301000-00015
Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg 1977; 59: 77–9. DOI: https://doi.org/10.2106/00004623-197759010-00013
Moreland JR. Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res 1988; 266: 49–64. DOI: https://doi.org/10.1097/00003086-198801000-00010
Boyd AD, Ewald FC, Thomas WH. Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am 1993; 75: 674. DOI: https://doi.org/10.2106/00004623-199305000-00006
Laskin RS. Flexion space configuration in total knee arthroplasty. J Arthroplasty 1995; 10: 657–60. DOI: https://doi.org/10.1016/S0883-5403(05)80211-6
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L. Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 2001; 392: 46–55.
Bellemans J, Vandenneucker H, Vanlauwe J. Robot-assisted total knee arthroplasty. Clin Orthop Relat Res 2007; 464: 111–6. DOI: https://doi.org/10.1097/BLO.0b013e318126c0c0
Liow MH, Chin PL, Tay KJ, Chia SL, Lo NN, Yeo SJ. Early experiences with robot-assisted total knee arthroplasty using the DigiMatch ROBODOC(R) surgical system. Singap Med J 2014; 55: 529–34. DOI: https://doi.org/10.11622/smedj.2014136
Song EK, Seon JK, Park SJ, Jung WB, Park HW, Lee GW. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 2011; 19: 1069–76. DOI: https://doi.org/10.1007/s00167-011-1400-9
Decking J, Theis C, Achenbach T, Roth E, Nafe B, Eckardt A. Robotic total knee arthroplasty: the accuracy of CT-based component placement. Acta Orthop Scand 2004; 75: 573–9. DOI: https://doi.org/10.1080/00016470410001448
Liow MH, Xia Z, Wong MK, Tay KJ, Yeo SJ, Chin PL. Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis. A prospective randomised study. J Arthroplasty 2014; 29: 2373–7. DOI: https://doi.org/10.1016/j.arth.2013.12.010
Siebert W, Mai S, Kober R, Heeckt PF. Technique and first clinical results of robot-assisted total knee replacement. Knee 2002; 9: 173–80. DOI: https://doi.org/10.1016/S0968-0160(02)00015-7
Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res 2013; 471: 118–26. DOI: https://doi.org/10.1007/s11999-012-2407-3
Coon TM. Integrating robotic technology into the operating room. Am J Orthop (Belle Mead NJ) 2009; 38(2 Suppl): 7–9.
Park SE, Lee CT. Comparison of roboticassisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty 2007; 22: 1054–9. DOI: https://doi.org/10.1016/j.arth.2007.05.036
Lonner JH, Smith JR, Picard F, Hamlin B, Rowe PJ, Riches PE. High degree of accuracy of a novel image-free handheld robot for unicondylar knee arthroplasty in a cadaveric study. Clin Orthop 2015; 473: 206–12. DOI: https://doi.org/10.1007/s11999-014-3764-x
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L. Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 2001; 392: 46–55. DOI: https://doi.org/10.1097/00003086-200111000-00006
Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 1998; 356: 144–53. DOI: https://doi.org/10.1097/00003086-199811000-00021
Berger RA, Rubash HE, Seel MJ, Warren HT, Crosset LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 1993; 286: 40–7. DOI: https://doi.org/10.1097/00003086-199301000-00008
Vince KG, Insall JN, Kelly MA. Total condylar prosthesis: 10- to 12-year results of a cemented knee replacement. J Bone Joint Surg Br 1989; 71-B: 793–7. DOI: https://doi.org/10.1302/0301-620X.71B5.2584249
Jeffery RS, Morris R, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br 1991; 73-B: 709–14. DOI: https://doi.org/10.1302/0301-620X.73B5.1894655
Jenny JY, Boeri C. Low reproducibility of the intra-operative measurement of the transepicondylar axis during total knee replacement. Acta Orthop Scand 2004: 75: 74-7. DOI: https://doi.org/10.1080/00016470410001708150
Liow MHL, Goh GS, Wong MK, Chin PL, Tay DK, Yeo SJ. Robotic assisted total knee arthroplasty may lead to improvement in quality of life measures: a 2 year follow up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 2017; 9: 2942-51. DOI: https://doi.org/10.1007/s00167-016-4076-3
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.