A REAL WORLD MANAGEMENT OF OSTEOARTHRITIS (OA) KNEE PATIENTS WHO UNDERGO TOTAL KNEE REPLACEMENT – A RETROSPECTIVE STUDY IN THAILAND. (ARMOR STUDY)
DOI:
https://doi.org/10.55374/jseamed.v2i1.23Keywords:
Total knee arthroplasty, Total knee replacement, Knee osteoarthritis, Pain managementAbstract
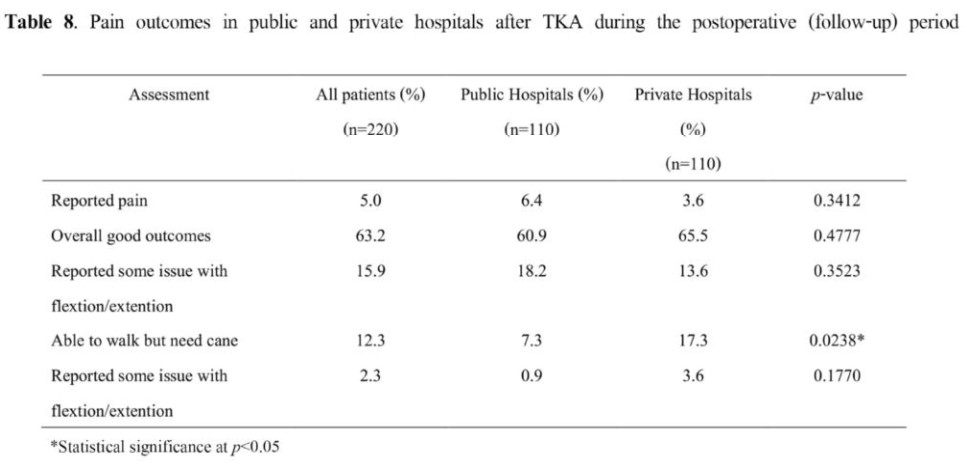
Background: In Thailand. Total knee replacement (TKA) is a common clinical intervention to manage patients with OA (osteoarthritis). Public and private hospitals tend to exhibit different patients of TKA use. Hence, knowledge with regard to TKA practice patterns, use and treatment outcomes in different hospitals in Thailand will improve the understanding of clinical management of OA and patient care. Objectives: The primary objective of the study was to examine the patterns of pain management during pre-operative, hospital admission for TKA, and postoperative periods (surgery to 3 months after discharge) for patients receiving TKA in public and private hospitals. The data were collected from various hospitals and subjected to analysis. Methods: This retrospective observational multi-center chart review study was conducted in public (n=2) and private (n=2) hospital in Thailand. A total of 220 patients diagnosed with knee OA (ICD-10 code, M17.0 and 17.1) who had undergone TKA were included in the study. The estimated ratio of patients from public and private hospitals was 1:1. Patient medical charts were accessed with the Ethics Committee’s approval. De-identified patient data were extracted from the chart and entered into a paper Case Report Form (CRF). Patients with history of major cardiovascular events and bilateral total knee replacement were excluded from the study. Results: At clinical baseline, cyclooxygenase-II (COX-II) inhibitors followed by traditional nonsteroidal anti-inflammatory drugs (tNSAIDs) were the preferred drug classes for pain management irrespective of hospital type or age group. At operation, use of pain control drugs was comparable between public and private hospitals. The use of concomitant drugs such as antithrombotic agents was observed to be frequent in both the hospital types and different age groups. After surgery, use of opioids was the highest among other drug classes followed by COX-II inhibitors and tNSAIDs; however, the use of opioids decreased faster daily compared with COX-II inhibitors which remained constant until 4 days after surgery. Among discharge pain control medications, analgesics and opiods were used extensively followed by COX-II inhibitors; however, the use of NSAIDs was very limited because of associated complications. During the follow-up period, opiods were the most commonly prescriped drug class in both hospital types; use of COX-II inhibitors was significantly higher in private hospitals The same trend of drug use was observed by age group (both > 70 and < 70 years of age). The proportion of patients with complications was observed more in public hospitals as compared with private settings. In the present study, patients receiving COX-II-inhibitors combined with other pain control medications reported lower pain scored than average after surgery. The clinical outcome distribution among patients receiving multiple pain control drugs during discharge was observed to be better compared with other combined regimens or analgesics alone. Conclusion: Pain management is one of the most important and challenging aspects of TKA. The patterns of pain management during pre-operative, during operation and postoperative stages differed. The use of COX-II inhibitors followed by NSAIDs was observed to be higher in the pre-operative stage, while use of opioids was higher after surgery and follow-up period compared with COX-II inhibitors
Downloads
Metrics
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.