DETERMINING STRESS AND ASSOCIATED FACTORS IN A RURAL COMMUNITY DURING COVID-19 PANDEMIC USING THE COVID STRESS SCALE
DOI:
https://doi.org/10.55374/jseamed.v6i0.133Keywords:
stress, COVID-19, COVID-stress scale, ruralAbstract
Background: The COVID-19 pandemic has affected people worldwide, both physically and mentally. Stress is one of the burdens being faced, especially in the working class. Therefore, this study aimed to explore and compare associated stress factors during the COVID-19 pandemic lockdown among adults in a rural community in Thailand using the COVID stress scale.
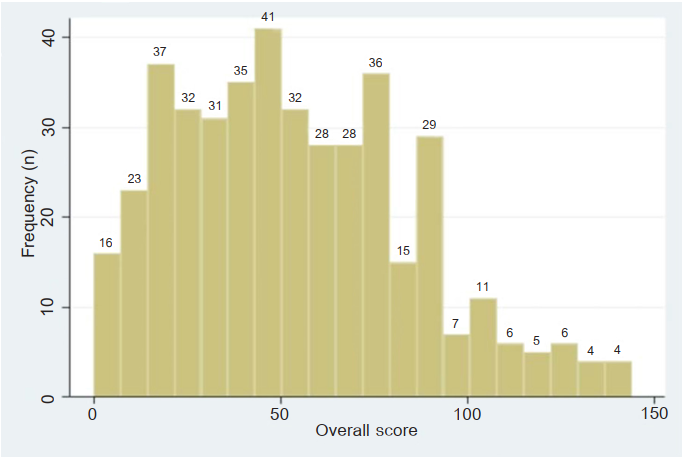
Methods: This cross-sectional study was conducted from December 2021 to March 2022 in Chachoengsao Province. It included adults aged 20 to 60 years old. The questionnaire included demographic data and the Thai COVID stress scale (T-CSS) version. The data were collected using face-to-face interviews. Associated factors of stress were assessed using linear regression.
Results: Data were compared with their counterparts, illiteracy (adjusted β=18.4, 95% CI 5.9-30.1) and agriculturists (adjusted β=13.2, 95% CI 3.1-23.4). At the same time, age 51-60 (adjusted β=-11.1, 95% CI 3.9-27.3) and vaccination with ≥3 doses of COVID-19 vaccine (adjusted β=-8.9, 95% CI -16.4 to -1.5) were associated with decreased stress level.
Discussion: Illiteracy and agriculturists were associated with higher stress scores. COVID-19 vaccination doses might affect stress levels due to the efficacy of preventing infection and severe illness. Older people had less stress due to better experience in stress management. Limitations included that T-CSS cannot determine the cut-off point of stress and nonstress in the population due to multiple factors. However, it might be possible to imply that outlier scores from a normal distribution are likely to be most stressful during the COVD-19 pandemic.
Downloads
Metrics
References
Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio Medica: Atenei Parmensis 2020; 91: 157.
Kunno J, Supawattanabodee B, Sumanasrethakul C, Wiriyasivaj B, Kuratong S, Kaewchandee C. Comparison of different waves during the COVID-19 pandemic: retrospective descriptive study in Thailand. Adv Prev Med 2021; 2021. DOI: https://doi.org/10.1155/2021/5807056
Kuai Y-H, Ser H-L. COVID-19 Situation in Thailand. Prog Biophys Mol 2021; 4.
Thanapluetiwong S, Chansirikarnjana S, Sriwannopas O, Assavapokee T, Ittasakul P. Factors associated with COVID-19 vaccine hesitancy in Thai seniors. Patient Prefer Adherence 2021; 15: 2389. DOI: https://doi.org/10.2147/PPA.S334757
Yoda T, Suksatit B, Tokuda M, Katsuyama H. Analysis of people’s attitude toward COVID-19 vaccine and Its information sources in Thailand. Cureus 2022; 14. DOI: https://doi.org/10.7759/cureus.22215
Sritipsukho P, Khawcharoenporn T, Siribumrungwong B, Damronglerd P, Suwantarat N, Satdhabudha A, et al. Comparing real-life effectiveness of various COVID-19 vaccine regimens during the delta variant-dominant pandemic: a test-negative case-control study. Emerg Microbes Infect 2022; 11: 585-92. DOI: https://doi.org/10.1080/22221751.2022.2037398
Shadmi E, Chen Y, Dourado I, Faran-Perach I, Furler J, Hangoma P, et al. Health equity and COVID-19: global perspectives. Int J Equity Health 2020; 19: 1-16. DOI: https://doi.org/10.1186/s12939-020-01218-z
Ghosh A, Gupta R, Misra A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: Guidelines for physicians Diabetes Metab Syndr 2021; 14: 273-76. DOI: https://doi.org/10.1016/j.dsx.2020.04.001
Intawong K, Olson D, Chariyalertsak S. Application technology to fight the COVID-19 pandemic: Lessons learned in Thailand. Biochem Biophys Res Commun 2021; 534: 830-36. DOI: https://doi.org/10.1016/j.bbrc.2020.10.097
Khan N, Jones D, Grice A, Alderson S, Bradley S, Carder P, et al. A brave new world: the new normal for general practice after the COVID-19 pandemic. BJGP open 2020; 4. DOI: https://doi.org/10.3399/bjgpopen20X101103
Nguyen HC, Nguyen MH, Do BN, Tran CQ, Nguyen TT, Pham KM, et al. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: the potential benefit of health literacy. J Clin Med 2020; 9: 965. DOI: https://doi.org/10.3390/jcm9040965
Yan Y, Malik AA, Bayham J, Fenichel EP, Couzens C, Omer SB. Measuring voluntary and policy-induced social distancing behavior during the COVID-19 pandemic. Proc Natl Acad Sci USA 2021; 118. DOI: https://doi.org/10.1073/pnas.2008814118
Mongkhon P, Ruengorn C, Awiphan R, Thavorn K, Hutton B, Wongpakaran N, et al. Exposure to COVID-19-related information and its association with mental health problems in Thailand: nationwide, cross-sectional survey study. J Med Internet Res 2021; 23: e25363. DOI: https://doi.org/10.2196/25363
Wang C, Tee M, Roy AE, Fardin MA, Srichokchatchawan W, Habib HA, et al. The impact of COVID-19 pandemic on physical and mental health of Asians: A study of seven middle-income countries in Asia. PLoS One 2021; 16: e0246824. DOI: https://doi.org/10.1371/journal.pone.0246824
Charoensakulchai S, Usawachoke S, Kongbangpor W, Thanavirun P, Mitsiriswat A, Pinijnai O, et al. Prevalence and associated factors influencing depression in older adults living in rural Thailand: A cross‐sectional study. Geriatr Gerontol Int 2019; 19: 1248-53. DOI: https://doi.org/10.1111/ggi.13804
Seangpraw K, Auttama N, Kumar R, Somrongthong R, Tonchoy P, Panta P. Stress and associated risk factors among the elderly: A cross-sectional study from rural Thailand. F1000Research 2019; 8. DOI: https://doi.org/10.12688/f1000research.17903.1
Chiu E. Epidemiology of depression in the Asia Pacific region. Australas Psychiatry 2004; 12: S4-S10. DOI: https://doi.org/10.1111/j.1039-8562.2004.02097.x-i1
Taylor S, Landry CA, Paluszek MM, Fergus TA, McKay D, Asmundson GJ. Development and initial validation of the COVID Stress Scales. J Anxiety Disord 2020; 72: 102232. DOI: https://doi.org/10.1016/j.janxdis.2020.102232
Tobacco glossary: Centers for Disease Control and Prevention; [Available from: https://www.cdc.gov/nchs/nhis/tobacco/tobacco_glossary.htm.
The Global Health Observatory: World Health Organization; 2022 [Available from: https://www.who.int/data/gho/indicator-metadata-registry.
Khademian F, Delavari S, Koohjani Z, Khademian Z. An investigation of depression, anxiety, and stress and its relating factors during COVID-19 pandemic in Iran. BMC Public Health 2021; 21: 1-7. DOI: https://doi.org/10.1186/s12889-021-10329-3
Torales J, Ríos-González C, Barrios I, O’Higgins M, González I, García O, et al. Self-perceived stress during the quarantine of COVID-19 pandemic in Paraguay: an exploratory survey. Front Psychiatr 2020; 11: 1155. DOI: https://doi.org/10.3389/fpsyt.2020.558691
Nwachukwu I, Nkire N, Shalaby R, Hrabok M, Vuong W, Gusnowski A, et al. COVID-19 pandemic: age-related differences in measures of stress, anxiety and depression in Canada. Int J Environ Res Public Health 2020; 17: 6366. DOI: https://doi.org/10.3390/ijerph17176366
Kowal M, Coll‐Martín T, Ikizer G, Rasmussen J, Eichel K, Studzińska A, et al. Who is the most stressed during the COVID‐19 pandemic? Data from 26 countries and areas. Appl Psychol Health Well-Being 2020; 12: 946-66. DOI: https://doi.org/10.1111/aphw.12234
Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020; 17: 1729. DOI: https://doi.org/10.3390/ijerph17051729
Taylor S. COVID stress syndrome: clinical and nosological considerations. Curr Psychiatry Rep 2021; 23: 1-7. DOI: https://doi.org/10.1007/s11920-021-01226-y
Liang L, Ren H, Cao R, Hu Y, Qin Z, Li C, et al. The effect of COVID-19 on youth mental health. Psychiatr Q 2020; 91: 841-52. DOI: https://doi.org/10.1007/s11126-020-09744-3
Monima LA, Usman IM, Kasozi KI, Aigbogun Jr EO, Bassey VA, Ifie J, et al. COVID-19 related mental health burdens: Impact of educational level and relationship status among low income earners of Western Uganda. Front Public Health 2020; 9: 739270. DOI: https://doi.org/10.21203/rs.3.rs-61564/v1
Do BN, Nguyen P-A, Pham KM, Nguyen HC, Nguyen MH, Tran CQ, et al. Determinants of health literacy and its associations with health-related behaviors, depression among the older people with and without suspected COVID-19 symptoms: a multi-institutional study. Front Public Health 2020; 8: 694. DOI: https://doi.org/10.3389/fpubh.2020.581746
Yang BX, Xia L, Huang R, Chen P, Luo D, Liu Q, et al. Relationship between eHealth literacy and psychological status during COVID‐19 pandemic: A survey of Chinese residents. J Nurs Manag 2021; 29: 805-12. DOI: https://doi.org/10.1111/jonm.13221
Sapbamrer R, Chittrakul J, Sirikul W, Kitro A, Chaiut W, Panya P, et al. Impact of COVID-19 pandemic on daily lives, agricultural working lives, and mental health of farmers in northern Thailand. Sustainability 2022; 14: 1189. DOI: https://doi.org/10.3390/su14031189
Chitra A, Gopinath R. A Study On Causes Of Stress To The Farmers During COVID-19 Pandemic. Int J Aquatic Sci 2021; 12: 773-82.
Birditt KS, Turkelson A, Fingerman KL, Polenick CA, Oya A. Age differences in stress, life changes, and social ties during the COVID-19 pandemic: Implications for psychological well-being. Gerontologist 2021; 61: 205-16. DOI: https://doi.org/10.1093/geront/gnaa204
Charles ST, Carstensen LL. Social and emotional aging. Annu Rev Psychol 2010; 61: 383-409. DOI: https://doi.org/10.1146/annurev.psych.093008.100448
World Health Organization. Interim recommendations for heterologous COVID-19 vaccine schedules: interim guidance, 16 December 2021. World Health Organization; 2021. DOI: https://doi.org/10.15557/PiMR.2020.0006
Yorsaeng R, Suntronwong N, Phowatthanasathian H, Assawakosri S, Kanokudom S, Thongmee T, et al. Immunogenicity of a third dose viral-vectored COVID-19 vaccine after receiving two-dose inactivated vaccines in healthy adults. Vaccine 2022; 40: 524-30. DOI: https://doi.org/10.1016/j.vaccine.2021.11.083
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.