PREVALENCE AND RISK FACTORS OF BLASTOCYSTIS SP. INFECTION AMONG PRIMARY SCHOOL CHILDREN IN A RURAL COMMUNITY, CENTRAL THAILAND
DOI:
https://doi.org/10.55374/jseamed.v1i2.32Keywords:
Blastocystis sp., cross-sectional study, parasitic infection, waterborne transmissionAbstract
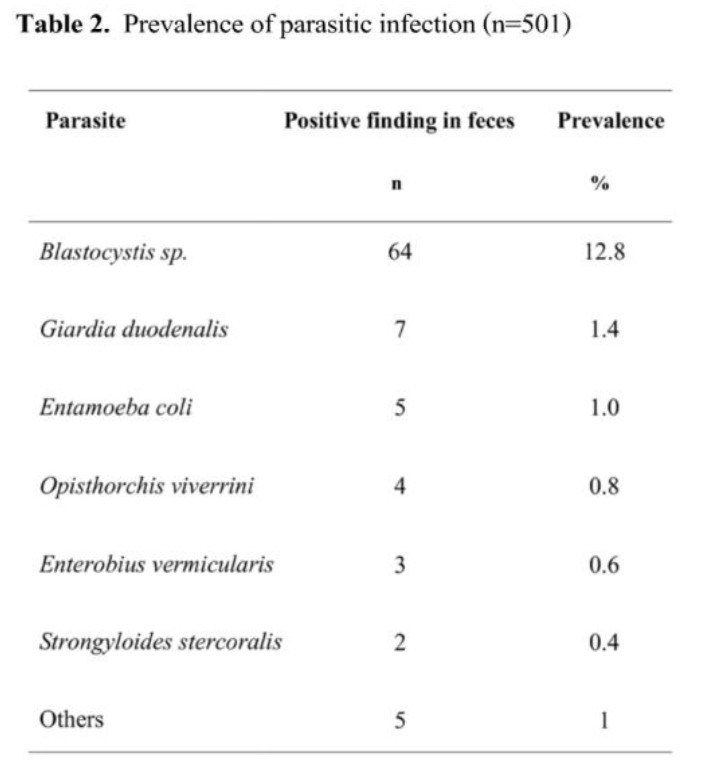
Background:Blastocystissp., a protozoan parasite, has been globally reported as one of the most common intestinal parasitic infections in humans. Water transmission plays an important role for the route of transmission of this organism to humans. Objectives:To determine the prevalence and risk factors of Blastocystissp.infection among schoolchildren in a rural community, central Thailand. Materials and Methods:In November 2015, schoolchildren from four primary schools (School A, B, C and D) at a rural community of Sanamchaikate district, Chacherngsao Province, central Thailand were enrolled into the study. Stool samples collected from participants were examined using wet preparation, phosphate buffered saline-ethyl acetate and Kato-Katz techniques. Short-term cultivation for Blastocystis sp. was performed using Jone’s medium supplemented with 10% horse serum. Strongyloides stercoralis was also detected using agar plate culture technique. Results:A total of 501 school children were analyzed. The mean age at diagnosis was 9.996±1.59years. The prevalence of overall parasitic infections was 17.8% and were diagnosed as follows: Blastocystis sp. in 64 participants (12.8%), Giardia duodenalis (1.4%), Entamoeba coli (1.0%), Opisthorchis viverrini(0.8%), Enterobius vermicuralis (0.6%), and Strongyloides stercolaris (0.4%). A significantly increased risk of Blastocystis sp.infection was found in children studying at the School B, C and A when compared with those studying at School D (p =0.001, OR =4.36, 95% CI =1.83-10.39, p =0.032, OR= 2.89,95% CI =1.10-7.64, and p =0.033, OR =2.2, 95% CI =1.06-4.54, respectively). Drinking water was suspected to be the source of transmission. However, screening by PCR at the 18S rRNA gene for Blastocystis sp. could not detect the parasites from any sources of drinking water samples collected from the four schools. Conclusion:Themost predominant intestinal protozoa infection in the study school children was Blastocystis sp. The high prevalence of protozoa infection could reflect the hygienic conditions of the children. Thus, health education and the control of intestinal parasitic infections are necessary to these children.
Downloads
Metrics
References
Stenzel DJ, Boreham PF. Blastocystis hominis revisited. Clin Microbiol Rev. 1996 Oct;9(4):563-84. DOI: https://doi.org/10.1128/CMR.9.4.563
Stensvold CR, Alfellani MA, Norskov-Lauritsen S, Prip K, Victory EL, Maddox C, Nielsen HV, Clark CG. Subtype distribution of Blastocystis isolates from synanthropic and zoo animals and identification of a new subtype. Int J Parasitol. 2009;39:473–479. DOI: https://doi.org/10.1016/j.ijpara.2008.07.006
Parkar U, Traub RJ, Vitali S, Elliot A, Levecke B, Robertson I, Geurden T, Steele J, Drake B, Thompson RC. Molecular characterization of Blastocystis isolates from zoo animals and their animal-keepers. Vet Parasitol. 2010;169:8–17. DOI: https://doi.org/10.1016/j.vetpar.2009.12.032
Stensvold CR, Suresh GK, Tan KS, Thompson RC, Traub RJ, Viscogliosi E, Yoshikawa H, Clark CG. Terminology for Blastocystis subtypes–a consensus. Trends Parasitol. 2007;23:93–96. DOI: https://doi.org/10.1016/j.pt.2007.01.004
Thathaisong U, Worapong J, Mungthin M, Tan-Ariya P, Viputtigul K, Sudatis A, Noonai A, Leelayoova S. Blastocystis isolates from a pig and a horse are closely related to Blastocystis hominis. J Clin Microbiol. 2003;41:967–975. DOI: https://doi.org/10.1128/JCM.41.3.967-975.2003
Tan KS. New insights on classification, identification, and clinical relevance of Blastocystis spp. Clin Microbiol Rev. 2008;21:639–665. DOI: https://doi.org/10.1128/CMR.00022-08
Leelayoova S, Siripattanapipong S, Thathaisong U, Naaglor T, Taamasri P, Piyaraj P, Mungthin M. Drinking water: a possible source of Blastocystis spp. subtype 1 infection in schoolchildren of a rural community in central Thailand. Am J Trop Med Hyg. 2008;79:401–406.
Parkar U, Traub RJ, Kumar S, Mungthin M, Vitali S, Leelayoova S, Morris K, Thompson RC. Direct characterization of Blastocystis from feces by PCR and evidence of zoonotic potential. Parasitology. 2007;134:359–367.
Boorom K., Smith H., Nimri L., Viscogliosi E., Spanakos G., Parkar U., et al. (2008) Oh my aching gut: irritable bowel syndrome, Blastocystis, and asymptomatic infection. Parasit Vectors 1: 40–40 DOI: https://doi.org/10.1186/1756-3305-1-40
Tan K., Mirza H., Teo J., Wu B., Macary P. (2010) Current views on the clinical relevance of Blastocystis spp. Curr Infect Dis Rep 12: 28–35 DOI: https://doi.org/10.1007/s11908-009-0073-8
Dogruman-Al F., Dagci H., Yoshikawa H., Kurt O., Demirel M. (2008) A possible link between subtype 2 and asymptomatic infections of Blastocystis hominis. Parasitol Res 103: 685–689 DOI: https://doi.org/10.1007/s00436-008-1031-3
Eroglu F., Genc A., Elgun G., Koltas I. (2009) Identification of Blastocystis hominis isolates from asymptomatic and symptomatic patients by PCR. Parasitol Res 105: 1589–1592 DOI: https://doi.org/10.1007/s00436-009-1595-6
Poirier P., Wawrzyniak I., Vivares C., Delbac F., El Alaoui H. (2012) New insights into Blastocystis spp.: a potential link with irritable bowel syndrome. PLoS Pathog 8: e1002545–e1002545 DOI: https://doi.org/10.1371/journal.ppat.1002545
Scanlan P.D. (2012) Blastocystis: past pitfalls and future perspectives. Trends Parasitol 28: 327–334 DOI: https://doi.org/10.1016/j.pt.2012.05.001
Leelayoova S, Rangsin R, Taamasri P, Naaglor T, Thathaisong U, Mungthin M. Evidence of waterborne transmission of Blastocystis hominis. Am J Trop Med Hyg. 2004;70(6):658–662. DOI: https://doi.org/10.4269/ajtmh.2004.70.658
Lee LI, Chye TT, Karmacharya BM, Govind SK. Blastocystis sp.: waterborne zoonotic organism, a possibility? Parasit Vectors. 2012 Jun 28;5:130. doi: 10.1186/1756-3305-5-130. DOI: https://doi.org/10.1186/1756-3305-5-130
Boondit J, Pipatsatitpong D, Mungthin M, Taamasri P, Tan-ariya P, Naaglor T, Leelayoova S. Incidence and risk factors of blastocystis infection in orphans at the Babies' Home, Nonthaburi Province, Thailand. J Med Assoc Thai. 2014 Feb;97 Suppl 2:S52-9.
Leelayoova S, Siripattanapipong S, Thathaisong U, Naaglor T, Taamasri P, Piyaraj P, Mungthin M. Drinking water: a possible source of Blastocystis spp. subtype 1 infection in schoolchildren of a rural community in central Thailand. Am J Trop Med Hyg. 2008 Sep;79(3):401-6. DOI: https://doi.org/10.4269/ajtmh.2008.79.401
Yoshikawa H, Wu Z, Pandey K, Pandey BD, Sherchand JB, Yanagi T, Kanbara H. Molecular characterization of Blastocystis isolates from children and rhesus monkeys in Kathmandu, Nepal. Vet Parasitol. 2009 Mar 23;160(3-4):295-300. doi: 10.1016/j.vetpar.2008.11.029. DOI: https://doi.org/10.1016/j.vetpar.2008.11.029
Wang W, Owen H, Traub RJ, Cuttell L, Inpankaew T, Bielefeldt-Ohmann H. Molecular epidemiology of Blastocystis in pigs and their in-contact humans in Southeast Queensland, Australia, and Cambodia. Vet Parasitol. 2014 Jul 14;203(3-4):264-9. doi: 10.1016/j.vetpar.2014.04.006. DOI: https://doi.org/10.1016/j.vetpar.2014.04.006
Belleza ML, Cadacio JL, Borja MP, Solon JA, Padilla MA, Tongol-Rivera PN, Rivera WL. Epidemiologic Study of Blastocystis Infection in an Urban Community in the Philippines. J Environ Public Health. 2015;2015:894297. doi: 10.1155/2015/894297. DOI: https://doi.org/10.1155/2015/894297
Warunee N, Choomanee L, Sataporn P, Rapeeporn Y, Nuttapong W, Sompong S, Thongdee S, Bang-On S, Rachada K. Intestinal parasitic infections among school children in Thailand. Trop Biomed. 2007 Dec;24(2):83-8.
Yaicharoen R, Ngrenngarmlert W, Wongjindanon N, Sripochang S, Kiatfuengfoo R. Infection of Blastocystis hominis in primary schoolchildren from Nakhon Pathom province, Thailand. Trop Biomed. 2006 Jun;23(1):117-22.
Ratanapo S, Mungthin M, Soontrapa S, Faithed C, Siripattanapipong S, Rangsin R, Naaglor T, Piyaraj P, Taamasri P, Leelayoova S. Multiple Modes of Transmission of Giardiasis in Primary Schoolchildren of a Rural Community, Thailand. Am J Trop Med Hyg. 2008 Apr;78(4):611-5 DOI: https://doi.org/10.4269/ajtmh.2008.78.611
Pipatsatitpong D, Leelayoova S, Mungthin M, Aunpad R, Naaglor T, Rangsin R. Prevalence and Risk Factors for Blastocystis Infection Among Children and Caregivers in a Child Care Center, Bangkok, Thailand. Am J Trop Med Hyg. 2015 Aug;93(2):310-5. DOI: https://doi.org/10.4269/ajtmh.14-0492
Coyle C., Varughese J., Weiss L., Tanowitz H. (2012) Blastocystis: to treat or not to treat. Clin Infect Dis 54: 105–110 DOI: https://doi.org/10.1093/cid/cir810
Nigro L., Larocca L., Massarelli L., Patamia I., Minniti S., Palermo F., et al. (2003) A placebo-controlled treatment trial of Blastocystis hominis infection with metronidazole. J Travel Med 10: 128–130 DOI: https://doi.org/10.2310/7060.2003.31714
Moghaddam D., Ghadirian E., Azami M. (2005) Blastocystis hominis and the evaluation of efficacy of metronidazole and trimethoprim/sulfamethoxazole. Parasitol Res 96: 273–275 DOI: https://doi.org/10.1007/s00436-005-1363-1
Stensvold C., Smith H., Nagel R., Olsen K., Traub R. (2010) Eradication of Blastocystis carriage with antimicrobials: reality or delusion? J Clin Gastroenterol 44: 85–90 DOI: https://doi.org/10.1097/MCG.0b013e3181bb86ba
Yoshikawa H, Abe N, Iwasawa M, Kitano S, Nagano I, Wu Z, Takahashi Y, 2000. Genomic analysis of Blastocystis hominis strains isolated from two long-term health care facilities. J Clin Microbiol 38: 1324--1330. DOI: https://doi.org/10.1128/JCM.38.4.1324-1330.2000
Mungthin M, Suwannasaeng R, Naaglor T, Areekul W, Leelayoova S, 2001. Asymptomatic intestinal microsporidiosis in Thai orphans and child-care workers. Trans R Soc Trop Med Hyg 95: 304–306 DOI: https://doi.org/10.1016/S0035-9203(01)90243-3
Taamasri P, Mungthin M, Rangsin R, Tongupprakarn B, Areekul W, Leelayoova S, 2000. Transmission of intestinal blastocystosis related to the quality of drinking water. Southeast Asian J Trop Med Public Health 31: 112–117.
Manganelli L, Berrilli F, Di Cave D, Ercoli L, Capelli G, Otranto D, Giangaspero A. Intestinal parasite infections in immigrant children in the city of Rome, related risk factors and possible impact on nutritional status. Parasit Vectors. 2012 Nov 20;5:265. doi: 10.1186/1756-3305-5-265. DOI: https://doi.org/10.1186/1756-3305-5-265
Waikagul J, Krudsood S, Radomyos P, Radomyos B, Chalemrut K, Jonsuksuntigul P, Kojima S, Looareesuwan S, Thaineau W. A cross-sectional study of intestinal parasitic infections among schoolchildren in Nan Province, Northern Thailand Southeast Asian J Trop Med Public Health. 2002 Jun;33(2):218-23.
Speich B, Marti H, Ame SM, Ali SM, Bogoch II, Utzinger J, Albonico M, Keiser J. Prevalence of intestinal protozoa infection among school-aged children on Pemba Island, Tanzania, and effect of single-dose albendazole, nitazoxanide and albendazole-nitazoxanide. Parasit Vectors. 2013 Jan 4;6:3. doi: 10.1186/1756-3305-6-3. DOI: https://doi.org/10.1186/1756-3305-6-3
Parkar U, Traub RJ, Kumar S, Mungthin M, Vitali S, Leelayoova S, Morris K, Thompson RC. Direct characterization of Blastocystis from faeces by PCR and evidence of zoonotic potential. Parasitology. 2007 Mar;134(Pt 3):359-67 DOI: https://doi.org/10.1017/S0031182006001582
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.