ASSOCIATION OF VITAMIN D LEVEL AND SEVERITY OF COVID-19 DISEASE
DOI:
https://doi.org/10.55374/jseamed.v8.202Keywords:
COVID-19, vitamin D deficiency, vitamin D insufficiency, COVID-19 severityAbstract
Background: Studies indicate that vitamin D can lower the incidence of viral respiratory infections and is necessary for the human immune system to function properly. Vitamin D deficiency may be a risk factor for the severity of COVID-19, including mortality, hospitalization, and length of hospital stay.
Objectives: This study aimed to investigate the association between vitamin D levels and the severity of COVID-19 disease.
Methods: The participants were COVID-19 patients aged 18 years or older who tested positive for the virus on Real-Time PCR tests, treated as inpatients at Banphaeo General Hospital between September 1 and November 30, 2021. For each patient, baseline characteristics, including sex, weight, height, and underlying diseases, were collected. Three categories were used to categorize COVID-19 disease: mild, moderate, and severe. At the beginning of the study, blood tests were performed on each patient to determine their 25-hydroxyvitamin D levels.
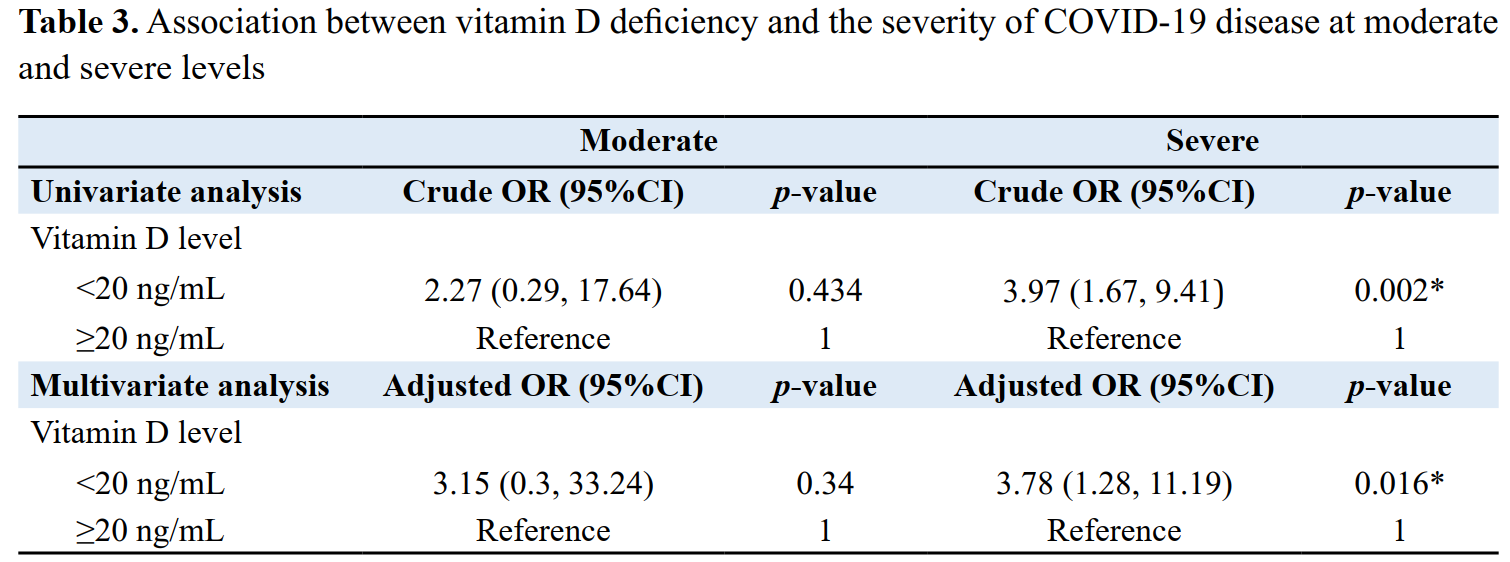
Results: Of 97 patients, 64 were male (66%), with a mean age of 50.8±17.7 years. The mean vitamin D level was 27.8±9.6 ng/mL, with 45 (46.4%) showing vitamin D deficiency and 39 (40.2%) indicating vitamin D insufficiency. Among COVID-19 patients with vitamin D deficiency, 28 (63.6%) were classified as severe, compared to only 16 severe cases (36.4%) among those without vitamin D deficiency, demonstrating statistically significant differences (p=0.006). Patients with vitamin D deficiency had a 3.97 times higher risk of experiencing severity (95% CI: 1.67, 9.41, p=0.002) than those without a vitamin D deficit. After adjusting for variable factors, results indicated that patients with vitamin D deficiency had a 3.78-fold increased risk of getting severe illness than those without deficiency (95% CI: 1.28, 11.19, p=0.016). Conclusion: These findings suggested that vitamin D deficiency was associated with the severity of COVID-19.
Downloads
Metrics
References
Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of Coronavirus disease 2019 (COVID-19): A review. JAMA 2020; 324: 782. DOI: https://doi.org/10.1001/jama.2020.12839
Wolff D, Nee S, Hickey NS, Marschollek M. Risk factors for Covid-19 severity and fatality: a structured literature review. Infection 2021; 49: 15–28. DOI: https://doi.org/10.1007/s15010-020-01509-1
D’Avolio A, Avataneo V, Manca A, Cusato J, De Nicolò A, Lucchini R, et al. 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2. Nutrients 2020; 12: 1359. DOI: https://doi.org/10.3390/nu12051359
Wang Z, Joshi A, Leopold K, Jackson S, Christensen S, Nayfeh T, et al. Association of vitamin D deficiency with COVID‐19 infection severity: Systematic review and meta‐ analysis. Clin Endocrinol (Oxf) 2022; 96: 281-7. DOI: https://doi.org/10.1111/cen.14540
Karatekin G, Kaya A, Salihoğlu Ö, Balci H, Nuhoğlu A. Association of subclinical vitamin D deficiency in newborns with acute lower respiratory infection and their mothers. Eur J Clin Nutr 2009; 63: 473–7. DOI: https://doi.org/10.1038/sj.ejcn.1602960
Dimitrov V, White JH. Species-specific regulation of innate immunity by vitamin D signaling. J Steroid Biochem Mol Biol 2016; 164: 246–53. DOI: https://doi.org/10.1016/j.jsbmb.2015.09.016
Sassi F, Tamone C, D’Amelio P. Vitamin D: Nutrient, hormone, and immunomodulator. Nutrients 2018; 10: 1656. DOI: https://doi.org/10.3390/nu10111656
Martineau AR, Jolliffe DA, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, et al. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis. Health Technol Assess 2019; 23: 1–44. DOI: https://doi.org/10.3310/hta23020
SACN. Update of rapid review: Vitamin D and acute respiratory tract infections. Accessed November11 2022. https://assetspublishingservicegovuk/government/uploads/system/uploads/attachment_data/file/945179/SACN_December2020_VitaminD_AcuteRespiratoryTractInfectionspdf.
Mercola J, Grant WB, Wagner CL. Evidence regarding vitamin D and risk of COVID-19 and its severity. Nutrients 2020; 12: 3361. DOI: https://doi.org/10.3390/nu12113361
Teshome A, Adane A, Girma B, Mekonnen ZA. The impact of vitamin D level on COVID-19 infection: Systematic review and meta-analysis. Front Public Health 2021; 9: 624559. DOI: https://doi.org/10.3389/fpubh.2021.624559
Shah K, Varna VP, Sharma U, Mavalankar D. Does vitamin D supplementation reduce COVID-19 severity?: a systematic review. QJM 2022; 115: 665–72. DOI: https://doi.org/10.1093/qjmed/hcac040
Ye K, Tang F, Liao X, Shaw BA, Deng M, Huang G, et al. Does serum vitamin D level affect COVID-19 infection and its severity? -A case-control study. J Am Coll Nutr 2021; 40: 724–31. DOI: https://doi.org/10.1080/07315724.2020.1826005
Siwamogsatham O, Ongphiphadhanakul B, Tangpricha V. Vitamin D deficiency in Thailand. J Clin Transl Endocrinol 2015; 2: 48–9. DOI: https://doi.org/10.1016/j.jcte.2014.10.004
COVID-19 Treatment Guidelines. National Institutes of Health (US). 2019; In: Coronavirus Disease 2019 (COVID-19)
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline. J Clin Endocrinol Metab 2011; 96: 1911–30. DOI: https://doi.org/10.1210/jc.2011-0385
Hossein-nezhad A, Holick MF. Vitamin D for health: A global perspective. Mayo Clin Proc 2013; 88: 720–55. DOI: https://doi.org/10.1016/j.mayocp.2013.05.011
Campi I, Gennari L, Merlotti D, Mingiano C, Frosali A, Giovanelli L, et al. Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy. BMC Infect Dis 2021; 21: 566. DOI: https://doi.org/10.1186/s12879-021-06281-7
Palacios C, Gonzalez L. Is vitamin D deficiency a major global public health problem? J Steroid Biochem Mol Biol 2014;n144: 138–45. DOI: https://doi.org/10.1016/j.jsbmb.2013.11.003
Chailurkit L-O, Aekplakorn W, Ongphiphadhanakul B. Regional variation and determinants of vitamin D status in sunshine-abundant Thailand. BMC Public Health 2011; 11: 853. DOI: https://doi.org/10.1186/1471-2458-11-853
Adami G, Rossini M, Bogliolo L, Cantatore FP, Varenna M, Malavolta N, et al. An exploratory study on the role of vitamin D supplementation in improving pain and disease activity in rheumatoid arthritis. Mod Rheumatol 2019; 29: 1059–62. DOI: https://doi.org/10.1080/14397595.2018.1532622
Rhodes JM, Subramanian S, Laird E, Griffin G, Kenny RA. Perspective: Vitamin D deficiency and COVID‐19 severity – plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis. J Intern Med 2021; 289: 97–115. DOI: https://doi.org/10.1111/joim.13149
Annweiler C, Hanotte B, Grandin de l’Eprevier C, Sabatier J-M, Lafaie L, Célarier T. Vitamin D and survival in COVID-19 patients: A quasi-experimental study. J Steroid Biochem Mol Biol 2020; 204: 105771. DOI: https://doi.org/10.1016/j.jsbmb.2020.105771
Nimitphong H, Holick MF. Vitamin D status and sun exposure in southeast Asia. Dermatoendocrinol 2013; 5: 34–7. DOI: https://doi.org/10.4161/derm.24054
Hansdottir S, Monick MM, Hinde SL, Lovan N, Look DC, Hunninghake GW. Respiratory epithelial cells convert inactive vitamin D to its active form: Potential effects on host defense. J Immunol 2008; 181: 7090–9. DOI: https://doi.org/10.4049/jimmunol.181.10.7090
Jiang J-S, Chou H-C, Chen C-M. Cathelicidin attenuates hyperoxia-induced lung injury by inhibiting oxidative stress in newborn rats. Free Radic Biol Med 2020; 150: 23–9. DOI: https://doi.org/10.1016/j.freeradbiomed.2020.02.005
Aranow C. Journal of investigative medicine : the official publication of the American Federation for Clinical Research 2011; 59 : 881–6. DOI: https://doi.org/10.2310/JIM.0b013e31821b8755
Hanff TC, Harhay MO, Brown TS, Cohen JB, Mohareb AM. Is there an association between COVID-19 mortality and the renin-angiotensin system? A call for epidemiologic investigations. Clin Infect Dis 2020; 71: 870–4. DOI: https://doi.org/10.1093/cid/ciaa329
Murai IH, Fernandes AL, Sales LP, Pinto AJ, Goessler KF, Duran CSC, et al. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: A randomized clinical trial. JAMA 2021; 325: 1053. DOI: https://doi.org/10.1001/jama.2020.26848
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.