COGNITIVE FUNCTIONS AMONG PATIENTS WHO RECOVERED FROM COVID-19
DOI:
https://doi.org/10.55374/jseamed.v7.145Keywords:
Postacute COVID-19, Cognitive impairment, MoCAAbstract
Introduction: The Coronavirus disease 2019 (COVID-19) spread, causing a worldwide pandemic and affecting multiple organs and systems. The possible long-term sequelae of COVID-19 have become an increasing concern. Currently, little information exists about prolonged COVID-19 affects related to cognitive functions.
Objective: The study aimed to investigate the cognitive functions of patients who recovered from COVID-19 at least three months after the diagnosis.
Methods: A cross-sectional study was conducted to investigate cognitive functions among 150 employees of Buddhasothorn Hospital, Chachoengsao, Thailand. Of these, 75 employees had a history of COVID-19 at least three months after the diagnosis. Demographic characteristics were recorded and screened for depression, anxiety and insomnia. They were tested for their cognitive functions using the Montreal Cognitive Assessment (MoCA) and compared with 75 employees without a history of COVID-19.
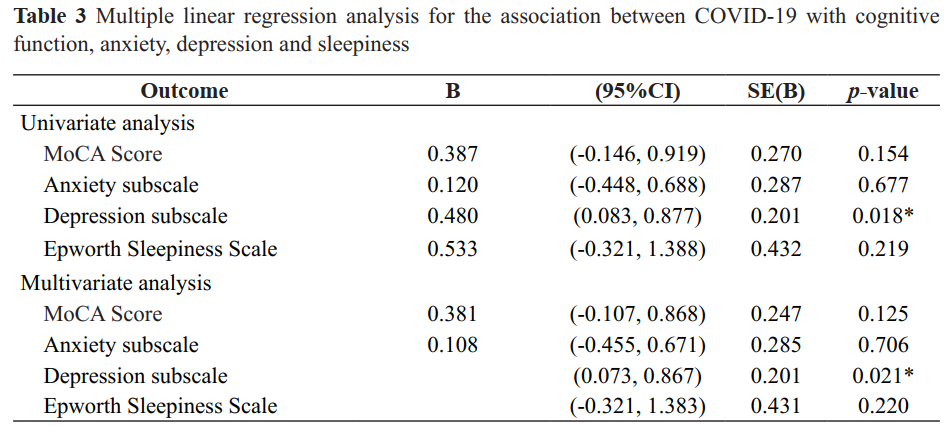
Results: All postCOVID-19 cases presented mild COVID-19 symptoms. The results showed that 96% of COVID-19 in both groups, cases and the healthy group, had normal cognitive functions using the MoCA that did not significantly differ. However, the depression score in the postCOVID-19 cases was significantly higher than that of the participants without a history of COVID-19 (1.09 ± 1.36 and 0.61 ± 1.09, respectively (p = 0.018). Regression analysis between the postCOVID-19 cases and depression using multivariate analysis showed that the postCOVID-19 cases were associated with depression scale (β coefficient=0.470; 95%CI: 0.073, 0.867, respectively), after adjusting for age, sex, educational level and underlying diseases.
Conclusion: The cognitive functions of employees having a history of COVID-19 and without infection did not differ.
Downloads
Metrics
References
WHO Director-General’s opening remarks at the media briefing on COVID19 -March 2020. https://www.youtube.com/watch?v=sbT6AANFOm4
Yong SJ. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis (Lond) 2021; 53: 737-54. DOI: https://doi.org/10.1080/23744235.2021.1924397
Lopez-Leon S, Wegman-Ostrosky T, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A, et al. More than 50 long-term effects of COVID-19: a systematic review and metaanalysis. SCi Rep 2021; 11: 16144. DOI: https://doi.org/10.1038/s41598-021-95565-8
Tavares-Junior JWL, de Souza ACC, Borges JWP, Oliveira DN, Siqueira-Neto JI, Sobreira-Neto MA, et al. COVID-19 associated cognitive impairment: A systematic review. Cortex 2022; 152: 77-97. DOI: https://doi.org/10.1016/j.cortex.2022.04.006
Writing Committee for the CSG, Morin L, Savale L, Pham T, Colle R, Figueiredo S, et al. Four-month clinical status of a cohort of patients after hospitalization for COVID-19. JAMA 2021; 325: 1525-34. DOI: https://doi.org/10.1001/jama.2021.3331
Del Rio C, Collins LF, Malani P. Long-term health consequences of COVID-19. JAMA 2020; 324: 1723-4. DOI: https://doi.org/10.1001/jama.2020.19719
Mattioli F, Stampatori C, Righetti F, Sala E, Tomasi C, De Palma G. Neurological and cognitive sequelae of Covid-19: a four month follow-up. J Neurol 2021; 268: 4422-8. DOI: https://doi.org/10.1007/s00415-021-10579-6
Nilchaikovit T, Lortrakul M, Phisansuthideth U. Development of Thai version of Hospital Anxiety and Depression Scale in cancer patients. J Psychiatr Assoc Thailand 1996; 41: 18-30.
Methipisit T, Mungthin M, Saengwanitch S, Ruangkana P, Chinwarun Y, Ruangkanchanasetr P, et al. The Development of Sleep Questionnaires Thai Version (ESS, SA-SDQ, and PSQI): linguistic validation, reliability analysis and cut-off level to determine sleep related problems in Thai population. J Med Assoc Thai 2016; 99: 893-903.
Tangwongchai S CT, Phannasathit M,, Akkayagorn L HS, Phanthumchinda, ZS KN. The Validity of Thai version of The Montreal Cognitive Assessment (MoCA - T). Dment Neuropsychol 2009; 3: 172.
Tenforde MW, Kim SS, Lindsell CJ, Billig Rose E, Shapiro NI, Files DC, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network - United States, March-June 2020. MMWR Morb Mortal Wkly Rep 2020; 69: 993-8. DOI: https://doi.org/10.15585/mmwr.mm6930e1
Daroische R, Hemminghyth MS, Eilertsen TH, Breitve MH, Chwiszczuk LJ. Cognitive Impairment After COVID-19-A Review on Objective Test Data. Front Neurol 2021; 12: 699582. DOI: https://doi.org/10.3389/fneur.2021.699582
Becker JH, Lin JJ, Doernberg M, Stone K, Navis A, Festa JR, et al. Assessment of Cognitive Function in Patients After COVID-19 Infection. JAMA Netw Open 2021; 4: e2130645. DOI: https://doi.org/10.1001/jamanetworkopen.2021.30645
Woo MS, Malsy J, Pottgen J, Seddiq Zai S, Ufer F, Hadjilaou A, et al. Frequent neurocognitive deficits after recovery from mild COVID-19. Brain Cummun 2020; 2: fcaa205. DOI: https://doi.org/10.1093/braincomms/fcaa205
Stavem K, Einvik G, Tholin B, Ghanima W, Hessen E, Lundqvist C. Cognitive function in non-hospitalized patients 8-13 months after acute COVID-19 infection: A cohort study in Norway. PLoS One 2022; 17: e0273352. DOI: https://doi.org/10.1371/journal.pone.0273352
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.