COMPARATIVE RANDOMIZED CONTROLLED STUDY OF ANALGESIC EFFECT BETWEEN ORAL COMBINATION ANALGESIA AND INTRAVENOUS ANALGESIA IN PATIENTS UNDERGOING EXTRACORPOREAL SHOCKWAVE LITHOTRIPSY AT PHRAMONGKUTKLAO HOSPITAL
DOI:
https://doi.org/10.55374/jseamed.v9.232Keywords:
ESWL, oral analgesia, KUB stone, Extracorporeal shockwave lithotripsy, Paracetamol, Ibuprofen, Tramadol, Fentanyl, Pain controlAbstract
Background: Extracorporeal Shockwave Lithotripsy (ESWL) is a widely used, noninvasive treatment for upper urinary tract stones. Despite its routine use, patients often experience significant pain during the procedure, and opioid-based analgesia such as intravenous fentanyl may lead to adverse effects. Optimizing pain control while minimizing opioid exposure remains a clinical challenge.
Objectives: To compare the analgesic efficacy and side effect profiles of three analgesic regimens during ESWL: intravenous fentanyl alone, a combination of oral and intravenous analgesics, and oral analgesics alone.
Methods: This randomized clinical trial included 78 ESWL sessions from 72 patients with renal or ureteric stones. Patients were randomized into three groups: Group A received intravenous fentanyl (50 µg); Group B received oral paracetamol (500 mg) and ibuprofen (400 mg) plus intravenous fentanyl (50 µg); Group C received oral tramadol (50 mg), paracetamol (500 mg), and ibuprofen (400 mg). A rescue dose of intravenous fentanyl 50 µg was offered when a patient reported an NRS score > 8 or was unable to tolerate the pain. The primary outcome was pain intensity, measured using the 11-point Numeric Rating Scale (NRS; 0 = no pain, 10 = worst possible pain), administered every 15 minutes during the procedure. Patients verbally rated their pain by choosing a number between 0 and 10. The secondary outcomes were the occurrence of adverse effects and the need for a rescue dose of intravenous fentanyl (50 µg, if NRS > 8 or intolerable pain). The stone-free rate was assessed at 2–4 weeks.
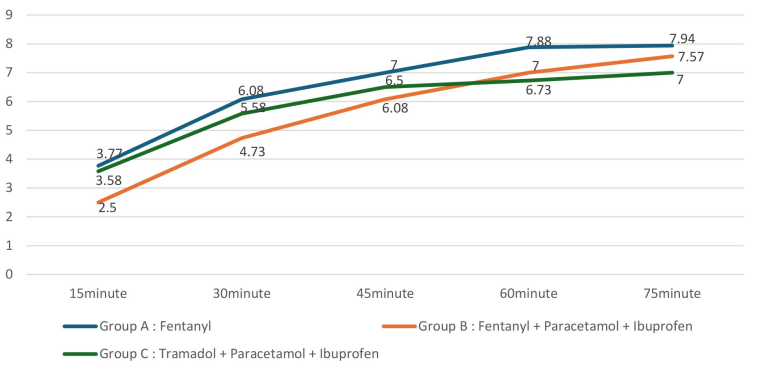
Results: Baseline characteristics were comparable between groups, except for body mass index. The mean pain scores were 6.39 ± 1.26 in Group A, 5.38 ± 1.85 in Group B, and 5.88 ± 1.34 in Group C. Group B reported significantly lower pain scores than Group A at 15 minutes (2.5 ± 1.96 vs. 3.77 ± 1.95, p = 0.018) and 30 minutes (4.73 ± 2.24 vs. 6.08 ± 1.81, p = 0.016). Group C had significantly lower pain scores at 60 minutes (6.73 ± 1.59 vs. 7.88 ± 1.99, p = 0.034) and 75 minutes (7 ± 1.39 vs. 7.94 ± 1.3, p = 0.040) compared to Group A. The incidence of adverse effects was lowest in Group C (dizziness: 23.1%). A rescue intravenous fentanyl dose was required among 6 (23.1%) of Group A, 6 (23.1%) of Group B, and 11 (42.3%) of Group C; these differences were not statistically significant.
Conclusion: Combining oral and intravenous analgesics offers superior early pain control during ESWL compared to intravenous fentanyl alone. Oral-only multimodal analgesia, with provision for a rescue intravenous fentanyl dose, administered when needed, provided comparable pain relief with fewer side effects and may reduce routine opioid use during ESWL. The inclusion and reporting of the rescue dose are essential for a consistent and practical analgesic strategy.
Downloads
Metrics
References
Chaussy C, Schuller JE, Schmiedt H, Brandl D, Jocham D, Liedl B. Extracorporeal shockwave lithotripsy (ESWL) for treatment of urolithiasis. Urology 1984; 23: 59–66. DOI: https://doi.org/10.1016/0090-4295(84)90243-7
Torrecilla Ortiz C, Rodríguez Blanco LL, Díaz Vicente F, González Satué C, Marco Pérez LM, Trilla Herrera E, et al. Extracorporeal shockwave lithotripsy: anxiety and pain perception. Actas Urol Esp 2000; 24: 163–8. Spanish. DOI: https://doi.org/10.1016/S0210-4806(00)72423-5
Knudsen F, Jorgensen S, Bonde J, Andersen JT, Mogensen P. Anesthesia and complications of extracorporeal shock wave lithotripsy of urinary calculi. J Urol 1992; 148: 1030–3. DOI: https://doi.org/10.1016/S0022-5347(17)36807-6
Alhashemi JA, Kaki AM. Anesthesiologistcontrolled versus patient-controlled propofol sedation for shockwave lithotripsy. Can J Anesth 2006; 53: 449–55. DOI: https://doi.org/10.1007/BF03022616
Bach C, Zaman F, Kachrilas S, Kumar P, Buchholz N, Masood J. Drugs for pain management in shock wave lithotripsy. Pain Res Treat 2011; 2011: 1–7. DOI: https://doi.org/10.1155/2011/259426
Akcali GE, Iskender A, Demiraran Y, Kayikci A, Yalcin GS, Cam K, et al. Randomized comparison of efficacy of paracetamol, lornoxicam, and tramadol representing three different groups of analgesics for pain control in extracorporeal shockwave lithotripsy. J Endourol 2010; 24: 615–20. DOI: https://doi.org/10.1089/end.2009.0483
Eker HE, Cok OY, Ergenoglu P, Aribogan A, Arslan G. IV paracetamol effect on propofol– ketamine consumption in paediatric patients undergoing ESWL. J Anesth 2012; 26: 351–6. DOI: https://doi.org/10.1007/s00540-012-1335-4
Cohen E, Hafner R, Rotenberg Z, Padilla M, Garty M. Comparison of ketorolac and diclofenac in the treatment of renal colic. Eur J Clin Pharmacol 1998; 54: 455–8. DOI: https://doi.org/10.1007/s002280050492
White PF. The changing role of non-opioid analgesic techniques in the management of postoperative pain. Anesth Analg 2005; 101(Suppl 5): S5–S22. DOI: https://doi.org/10.1213/01.ANE.0000177099.28914.A7
Varrassi G, Müller-Schwefe G, Pergolizzi J, Orónska A, Morlion B, Mavrocordatos P, et al. Pharmacological treatment of chronic pain—the need for CHANGE. Curr Med Res Opin 2010; 26: 1231–45. DOI: https://doi.org/10.1185/03007991003689175
Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain 2016; 17: 131–57. DOI: https://doi.org/10.1016/j.jpain.2015.12.008
Sinatra RS. Role of COX-2 inhibitors in the evolution of acute pain management. J Pain Symptom Manage 2002; 24(1 Suppl): S18–27. DOI: https://doi.org/10.1016/S0885-3924(02)00410-4
Romsing J, Moiniche S. A systematic review of COX-2 inhibitors compared with traditional NSAIDs, or different COX-2 inhibitors for postoperative pain. Acta Anaesthesiol Scand 2004; 48: 525–46. DOI: https://doi.org/10.1111/j.0001-5172.2004.00379.x
Fredman B, Jedeikin R, Olsfanger D, Aronheim M. The opioid-sparing effect of diclofenac sodium in outpatient extracorporeal shock wave lithotripsy (ESWL). J Clin Anesth 1993; 5: 141–4. DOI: https://doi.org/10.1016/0952-8180(93)90142-2
Choudhary A, Basu S, Sharma R, Gupta R, Das RK, Dey RK. A novel triple oral regimen provides effective analgesia during extracorporeal shockwave lithotripsy for renal stones. Urol Ann 2019; 11: 66–71. DOI: https://doi.org/10.4103/UA.UA_15_18
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.