DIAGNOSIS OF IRON DEFICIENCY ANEMIA IN THAI FEMALE ADOLESCENTS USING RETICULOCYTE HEMOGLOBIN EQUIVALENT
DOI:
https://doi.org/10.55374/jseamed.v6i0.126Keywords:
Iron deficiency anemia, Reticulocyte, Hemoglobin, Reticulocyte hemoglobin equivalent, Thai female adolescentsAbstract
Background: Female adolescents aged 10 to 19 years are at remarkable risk of iron deficiency anemia (IDA). Reticulocyte hemoglobin equivalent (Ret-He) is an initial indicator of iron incorporation in red blood cells (RBCs) hemoglobin and reflects the iron functional availability in the RBCs.
Objective: This study aimed to assess the diagnostic performance of Ret-He to identify IDA and determine a specific cut-off value for Thai female adolescents.
Methods: Blood samples of 191 Thai female adolescents, ages ranging from 12 to 18 years, were included. Patients underwent complete blood count, reticulocyte count, Ret-He, serum iron (SI), total iron-binding capacity (TIBC), and transferrin saturation (TSAT). The correlation of Ret-He with other parameters and the diagnostic performance to identify IDA were evaluated.
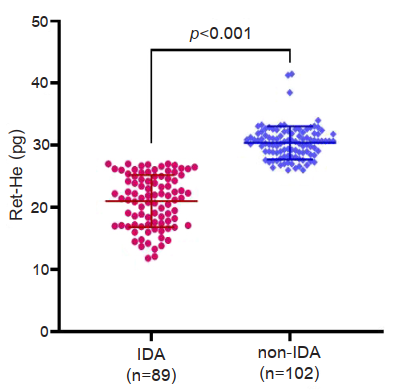
Results: Among 191 patients, 89 and 102 were defined as IDA and non-IDA groups. Ret-He value in the IDA group was significantly lower than that in the non-IDA group (p<0.001). Strong positive correlations were observed between Ret-He and RBC indices and SI and TSAT (p<0.001). A Ret-He value of ≤27.0 pg could distinguish IDA from non-IDA with a sensitivity of 91.2% and a specificity of 100.0% (area under the curve, AUC of 0.99, 95% CI: 0.98-0.99; p<0.001).
Conclusion: This study confirmed that Ret-He is a cost-effective parameter representing an advantage over other traditional iron markers. A specific Ret-He cut-off value of ≤27.0 pg is suitable for distinguishing IDA from non-IDA with excellent diagnostic performance among Thai female adolescents.
Downloads
Metrics
References
Ennis KM, Dahl LV, Rao RB, Georgieff MK. Reticulocyte hemoglobin content as an early predictive biomarker of brain iron deficiency. Pediatr Res 2018; 84: 765-79. DOI: https://doi.org/10.1038/s41390-018-0178-6
Speeckaert MM, Speeckaert R, Delanghe JR. Biological and clinical aspects of soluble transferrin receptor. Crit Rev Clin Lab Sci 2010; 47: 213-28. DOI: https://doi.org/10.3109/10408363.2010.550461
Murray-Kolb LE, Beard JL. Iron treatment normalizes cognitive functioning in young women. Am J Clin Nutr 2007; 85: 778-87. DOI: https://doi.org/10.1093/ajcn/85.3.778
Devaki PB, Chandra RK, Geisser P. Effects of oral iron (III) hydroxide polymaltose complex supplementation on hemoglobin increase, cognitive function, affective behavior and scholastic performance of adolescents with varying iron status: A single centre proscentere placebo controlled study. Arzneimittelforschung 2009; 59: 303-10. DOI: https://doi.org/10.1055/s-0031-1296401
Fucharoen S, Winichagoon P, Siritanaratkul N, Chowthaworn J, Pootrakul P. Alpha- and beta-thalassemia in Thailand. Ann N Y Acad Sci 1998; 850: 412-4. DOI: https://doi.org/10.1111/j.1749-6632.1998.tb10507.x
Kittisares K, Palasuwan D, Noulsri E, Palasuwan A. Thalassemia trait and G6PD deficiency in Thai blood donors. Transfus Apher Sci 2019; 58: 201-6. DOI: https://doi.org/10.1016/j.transci.2019.03.009
Viprakasit V, Ekwattanakit S. Clinical classification, screening and diagnosis for thalassemia. Hematol Oncol Clin North Am 2018; 32: 193-211. DOI: https://doi.org/10.1016/j.hoc.2017.11.006
Munkongdee T, Chen P, Winichagoon P, Fucharoen S, Paiboonsukwong K. Update in laboratory diagnosis of thalassemia. Front Mol Biosci 2020; 7: 74. DOI: https://doi.org/10.3389/fmolb.2020.00074
Brugnara C, Schiller B, Moran J. Reticulocyte hemoglobin equivalent (Ret He) and assessment of iron-deficient states. Clin. Lab. Haematol 2006; 28: 303-8. DOI: https://doi.org/10.1111/j.1365-2257.2006.00812.x
Dalimunthe NN, Lubis AR. Usefulness of reticulocyte hemoglobin equivalent in management of regular hemodialysis patients with iron deficiency anemia. Rom J Intern Med 2016; 54: 31-6. DOI: https://doi.org/10.1515/rjim-2016-0003
Toki Y, Ikuta K, Kawahara Y, Niizeki N, Kon M, Enomoto M et al. Reticulocyte hemoglobin equivalent as a potential marker for diagnosis of iron deficiency. Int J Hematol 2017; 106: 116-25. DOI: https://doi.org/10.1007/s12185-017-2212-6
Auerbach M, Staffa SJ, Brugnara C. Using reticulocyte hemoglobin equivalent as a marker for iron deficiency and responsiveness to iron therapy. Mayo Clin Proc 2021; 96: 1510-9. DOI: https://doi.org/10.1016/j.mayocp.2020.10.042
Sanyoto A, Suega K, Adnyana L, Bakta IM. Diagnostic test equivalent hemoglobin reticulocyte in iron deficiency anemia. Indones Biomed J 2017; 9: 143. DOI: https://doi.org/10.18585/inabj.v9i3.267
Sunkara A, Kotta D. Evaluation of red cell indices and reticulocyte maturity indices including reticulocyte haemoglobin concentration in iron deficiency anaemia adult female population. J Evid Based Med Healthc 2016; 3: 5315-8. DOI: https://doi.org/10.18410/jebmh/2016/1105
Davidkova S, Prestidge TD, Reed PW, Kara T, Wong W, Prestidge C. Comparison of reticulocyte hemoglobin equivalent with traditional markers of iron and erythropoiesis in pediatric dialysis. Pediatr Nephrol 2016; 31: 819-26. DOI: https://doi.org/10.1007/s00467-015-3284-2
Miwa N, Akiba T, Kimata N, Hamaguchi Y, Arakawa Y, Tamura T. et al. Usefulness of measuring reticulocyte hemoglobin equivalent in the management of haemodialysis patients with iron deficiency. Int J Lab Hematol 2010; 32: 248-55. DOI: https://doi.org/10.1111/j.1751-553X.2009.01179.x
Semmelrock M, Raggam R, Amrein K, Avian A, Schallmoser K, Lanzer G. et al. Reticulocyte hemoglobin content allows early and reliable detection of functional iron deficiency in blood donors. Clinica Chimica Acta 2012; 413: 678-82. DOI: https://doi.org/10.1016/j.cca.2011.12.006
Brugnara C, Zurakowski D, DiCanzio J, Boyd T, Platt O. Reticulocyte hemoglobin content to diagnose iron deficiency in children. JAMA 1999; 281: 2225-30. DOI: https://doi.org/10.1001/jama.281.23.2225
Wirawan R, Tedja AT, Henrika F, Lydia A. Concordance between reticulocyte hemoglobin equivalent and reticulocyte hemoglobin content in CKD patients undergoing hemodialysis. Acta Medica Indonesiana 2017; 49: 34-40.
Chaipokam J, Na Nakorn T, Rojnuckarin P. Diagnostic accuracy of reticulocyte hemoglobin content in Thai patients with microcytic red cells as a test for iron deficiency anemia. Asian Biomed 2017; 10(s1): s31-7.
Kadegasem P, Songdej D, Lertthammakiat S, Chuansamrit A, Paisooksantivatana K, Mahaklan L. et al. Reticulocyte hemoglobin equivalent in a thalassemia-prevalent area. Pediatr Int 2019; 61: 240-5. DOI: https://doi.org/10.1111/ped.13775
Chinudomwong P, Binyasing A, Trongsakul R, Paisooksantivatana K. Diagnostic performance of reticulocyte hemoglobin equivalent in assessing the iron status. J Clin Lab Anal 2020; 34: e23225. DOI: https://doi.org/10.1002/jcla.23225
Ekplakorn W. The 6th Thai people’s health survey by physical examination (2013). Health Systems Research Institute (HSRI). http://www.thaincd.com/document/file/info/non-communicable-disease. Accessed on June 20, 2020.
World Health Organization. Iron deficiency anaemia: Assessment, prevention, and control. In: A guide for programme managers. Geneva: WHO/NHD/01.3; 2001; 2001
Beutler E, Hoffbrand AV, Cook JD. Iron deficiency and overload. Hematology Am Soc Hematol Educ Program. 2003:40-61 DOI: https://doi.org/10.1182/asheducation-2003.1.40
Schoorl M, Schoorl M, van der Gaag D, Bartels PCM. Effects of iron supplementation on red blood cell hemoglobin content in pregnancy. Hematol Rep 2012; 4: e24. DOI: https://doi.org/10.4081/hr.2012.e24
Bó SD, Fragoso ALR, Farias MG, Hubner DPG, de Castro SM. Evaluation of RET-He values as an early indicator of iron deficiency anemia in pregnant women. Hematol Transfus Cell Ther 2021: S2531-1379(21)00089-4. DOI: https://doi.org/10.1016/j.htct.2021.05.006
Levy S, Schapkaitz E. The clinical utility of new reticulocyte and erythrocyte parameters on the Sysmex XN 9000 for iron deficiency in pregnant patients. Int J Lab Hematol 2018; 40: 683-90. DOI: https://doi.org/10.1111/ijlh.12904
Uçar MA, Falay M, Dağdas S, Ceran F, Urlu SM, Özet G. The importance of RET-He in the diagnosis of iron deficiency and iron deficiency anemia and the evaluation of response to oral iron therapy. J Med Biochem 2019; 38: 496-502. DOI: https://doi.org/10.2478/jomb-2018-0052
Salam S, Hassane B, Koulidiati J, Koumpingnin N, Abou C, Abdoul-Guaniyi S. et al. Added-value of reticulocyte haemoglobin equivalent in the early diagnosis of iron deficiency states among blood donors: A pilot study in Burkina Faso. Health Sci Dis 2020; 21: 1-8.
Knovich MA, Storey JA, Coffman LG, Torti SV, Torti FM. Ferritin for the clinician. Blood Rev 2009; 23: 95-104. DOI: https://doi.org/10.1016/j.blre.2008.08.001
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.