FREQUENCIES OF PREDICTED MIA ANTIGEN AMONG SOUTHERN THAI BLOOD DONORS
DOI:
https://doi.org/10.55374/jseamed.v6i0.107Keywords:
Genotyping, MNS blood group system, Predicted Mi(a ) frequency, Southern ThaisAbstract
Background: The Mia antigen (MNS7) of the MNS blood group system is clinically important in Asian populations. Anti-Mia has been implicated in hemolytic transfusion reactions and hemolytic disease of the fetus and newborn in Thai populations. However, data of this antigen frequency among southern Thais remains unknown.
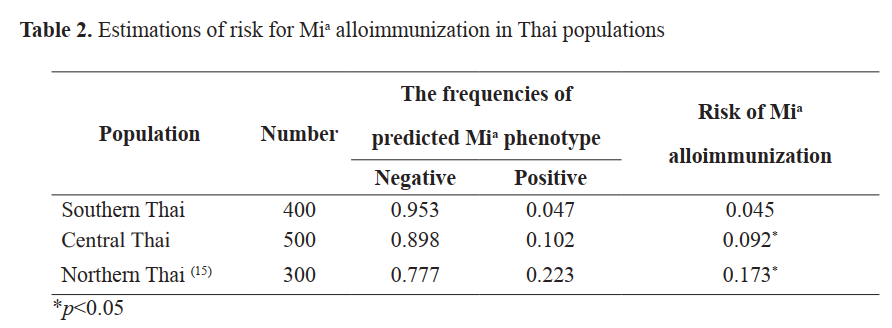
Objective: This study aimed to determine and predict Mia antigen frequencies among southern Thai blood donors and to estimate the risk of alloimmunization among Thais.
Methods: A cross-sectional study was conducted. Altogether, 400 southern and 500 central Thai blood samples were genotyped for GYP(B-A-B) and GYP(A-B-A) MNS hybrids using polymerase chain reaction with sequence-specific primer (PCR-SSP).
Results: Among them, 19 of 400 (4.45%), and 28 of 500 (9.33%) were positive with the set of GP. Hut, GP.HF, GP.Mur, GP.Hop, and GP.Bun. No GP.Vw phenotype was found among southern and central Thais. The predicted Mi(a+)frequency among southern Thais was significantly lower than among central and northern Thais (p<0.05). Its frequency was similar to Vietnamese, Taiwanese, and Southern Han Chinese populations (p>0.05) but significantly differed from Indonesian, Filipino, and Chinese (Guangzhou) populations (p<0.05). The risk of Mia alloimmunization among southern Thais was significantly lower than among both Thai groups (p<0.05).
Conclusion: This constitutes the first study to report Mi(a+) frequencies among southern Thais, supporting the estimation risk of alloimmunization and providing transfusion safety among Thai populations.
Downloads
Metrics
References
Cleghorn TE. A memorandum on the Miltenberger blood groups. Vox Sang 1966; 1: 219-22. DOI: https://doi.org/10.1159/000465106
Daniels G. Human blood groups, 3rd ed. Malden, MA, Blackwell Science, 2013. DOI: https://doi.org/10.1002/9781118493595
Reid ME, Lomas-Francis C, Olsson M. The blood group antigen factsbook, 3rd ed. New York, Academic Press, 2012. DOI: https://doi.org/10.1016/B978-0-12-415849-8.00026-0
Lopez GH, Wilson B, Turner RM, Millard GM, Roots NM, Liew YW, et al. Frequency of Mia (MNS7) and classification of Mia-positive hybrid glycophorins in an Australian blood donor population. Transfus Med Hemother 2020; 47: 279-86. DOI: https://doi.org/10.1159/000504026
Makroo RN, Bhatia A, Chowdhry M, Rosamma NL, Karna P. Frequency of Mi(a) antigen: A pilot study among blood donors. Indian J Med Res 2016; 143: 63-5. DOI: https://doi.org/10.4103/0971-5916.187112
Chandanyingyong D, Pejrachandra S. Studies on the Miltenberger complex frequency in Thailand and family studies. Vox Sang 1965; 28: 152-5. DOI: https://doi.org/10.1159/000466818
Chen V, Halverson G, Wasniowska K, Lisowska E, Chen J, Moulds M, Reid ME. Direct evidence for the existence of Miltenberger antigen. Vox Sang 2001; 80: 230-3. DOI: https://doi.org/10.1046/j.1423-0410.2001.00042.x
Chiewsilp P, Yodpornpin W, Cherdchai S. Delayed hemolytic transfusion reaction due to anti-Mia [in Thai]. Thai J Hematol Transfus 1996; 6: 289-90.
Lin M, Broadberry RE. An intravascular hemolytic transfusion reaction due to anti- ′Mi(a)′ in Taiwan. Vox Sang 1994; 67: 320. DOI: https://doi.org/10.1159/000462625
Cheng G, Hui CH, Lam CK, Hal SY, Wong L, Mak KH, Lin CK. Haemolytic transfusion reactions due to Mi-antibodies; need to include MiltenbergerIII positive cells in pre-transfusion antibody screening in Hong Kong. Clin Lab Haematol 1995; 17: 183-4.
Lin CK, Mak KH, Szeto SC, Poon KH, Yuen CMY, Chan NK, et al. First case of haemolytic disease of the newborn due to anti-Mur in Hong Kong. Clin Lab Haematol 1996; 18: 19-22. DOI: https://doi.org/10.1111/j.1365-2257.1996.tb00731.x
Wu KH, Chang JG, Lin M, Shih MC, Lin HC, Lee CC, et al. Hydrops foetalis caused by anti-Mur in first pregnancy--a case report. Transfus Med 2002; 12: 325-7. DOI: https://doi.org/10.1046/j.1365-3148.2002.00394.x
Prathiba R, Lopez CG, Usin FM. The prevalence of GP Mur and anti- ″Mia″ in a tertiary hospital in Peninsula Malaysia. Malays J Pathol 2002; 24: 95-8.
Palacajornsuk P, Nathalang O, Tantimavanich S, Bejrachandra S, Reid ME. Detection of MNS hybrid molecules in the Thai population using PCR-SSP technique. Transfus Med 2007; 17: 169-74. DOI: https://doi.org/10.1111/j.1365-3148.2007.00747.x
Intharanut K, Bejrachandra S, Nathalang S, Leetrakool N, Nathalang O. Red cell genotyping by multiplex PCR identifies antigen-matched blood units for transfusion-dependent Thai patients. Transfus Med Hemother 2017; 44: 358-64. DOI: https://doi.org/10.1159/000471886
K, Lin YC, Chao HP, Lee TY, Lin M, Chan YS. Assessing the frequencies of GP.Mur (Mi.III) in several Southeast Asian populations by PCR typing. Transfus Apher Sci 2013; 49: 370-1. DOI: https://doi.org/10.1016/j.transci.2013.05.011
Wei L, Lopez GH, Zhang Y, Wen J, Wang Z, Fu Y, et al. Genotyping analysis of MNS blood group GP(B-A-B) hybrid glycophorins in the Chinese Southern Han population using a high-resolution melting assay. Transfusion 2018; 58: 1763-71. DOI: https://doi.org/10.1111/trf.14641
Wei L, Shan ZG, Flower RL, Wang Z, Wen JZ, Luo GP, et al. The distribution of MNS hybrid glycophorins with Mur antigen expression in Chinese donors including identification of a novel GYP.Bun allele. Vox Sang 2016; 111: 308-14. DOI: https://doi.org/10.1111/vox.12421
Nathalang O. Red cell genotyping in Thailand: trends for blood transfusion in Asian populations. VOXS 2020; 15: 310-4. DOI: https://doi.org/10.1111/voxs.12547
Promwong C, Siammai S, Hassarin S, Buakaew J, Yeela T, Soisangwan P, et al. Frequencies and specificities of red cell alloantibodies in the Southern Thai population. Asian J Transfus Sci 2013; 7: 16-20. DOI: https://doi.org/10.4103/0973-6247.106718
Kupatawintu P, Emthip M, Sungnoon D, O-vataga P, Manakul V, Limtamaporn S, et al. Unexpected antibodies of patients, blood samples sent for testing at NBC. TRCS [in Thai]. J Hematol Transfus Med 2010; 20: 255-62.
Fucharoen S, Tanphaichitr VS, Torcharus K, Viprakasit V, Mekaewkunchorn A: Clinical practice guidelines for diagnosis and management of thalassemia syndromes. 1sted, (in Thai) Bangkok, P.A. Living, 2014.
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.