THE PSYCHOLOGICAL IMPACT AND COPING AMONG MEDICAL STUDENTS IN PHRAMONGKUTKLAO COLLEGE OF MEDICINE DURING THE COVID-19 PANDEMIC
DOI:
https://doi.org/10.55374/jseamed.v6i0.106Keywords:
psychological impact, Covid-19, coping, medical cadets and medical students, Phramongklao College of medicine (PCM)Abstract
Background: The COVID-19 pandemic has impacted on medical education and other areas of life causing psychological distress.
Objectives: The study aimed to assess psychological impact and coping and to identify factors associated psychological impact among medical students.
Methods: An online cross-sectional study was conducted at Phramongkutklao College of Medicine (PCM) in April 2021. All medical students were invited to complete a standardized online questionnaire for demographics data, impact of COVID-19, coping, fear of illness and virus evaluation (FIVE). The Depression Anxiety Stress Scales (DASS-21) Thai version was used to assess the psychological impact. The factors associated with depression, anxiety and stress were analyzed using logistic regression analysis.
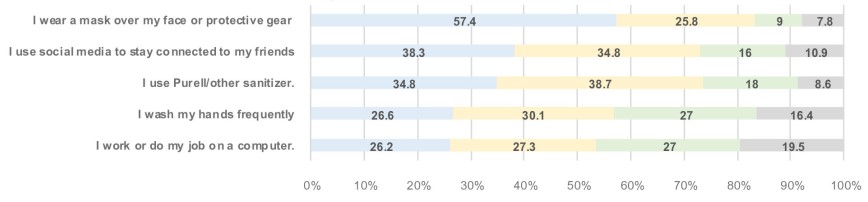
Results: In total, 256 medical students completed the questionnaire. Of these, 54.7% reported having psychological impact, 43.4% depression, 36.7% anxiety and 29.7% stress. Depression was associated with preclinical students (adjusted OR(AOR) =3.03, 95% confidence interval (95% CI) =1.54-5.97), sleep problem (AOR =2.20, 95% CI=1.16-4.16) and extreme deterioration of family income (AOR =7.27, 95% CI=1.81-29.29). Anxiety was associated with preclinical students (AOR =3.20, 95% CI=1.52-6.72), COVID-19 like symptoms (AOR =2.93, 95% CI=1.26-6.83), slight problems adjusting to new learning methods (AOR =6.11, 95% CI=1.54-24.24) and extreme deterioration of family income (AOR =8.29, 95% CI=1.44-47.59). Stress was associated with preclinical students (AOR =3.84, 95% CI=1.75-8.40), COVID-19-like symptoms (AOR =3.54, 95% CI=1.53-8.19), and no confidence in COVID-19 policy of PCM (AOR =2.3, 95% CI=1.06-4.98). A positive correlation between Fear of Illness and Virus Evaluation (FIVE) and psychological impact was observed (r=0.449; p<0.001). Common coping activities were the use of social media, video chats and exercise.
Conclusion: A high prevalence of psychological impact was observed among medical students during the COVID-19 pandemic. To establish psychological support and resilience, training is needed to improve mental wellbeing and prepare medical students to cope with unprecedented situations.
Downloads
Metrics
References
World Health Organization. Coronavirus Disease (COVID-2019) Situation Reports; WHO: Geneva, Switzerland,2020; Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/(accessed on 4 May 2020)
WHO Coronavirus (COVID-19) Dashboard [Internet]. Covid19.who.int 2021 [cited 5 May 2021]. Available from: https://covid19.who.int/
COVID-19 situation reports [Internet]. Covid19.ddc.moph.go.th 2021 [cited 5 May 2021]. Available from: https://covid19.ddc.moph.go.th/
Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet 2020; 395: e37-e38. DOI: https://doi.org/10.1016/S0140-6736(20)30309-3
Hope V, Henderson M. Medical student depression, anxiety and distress outside North America: a systematic review. Med Ed 2014; 48: 963-79. DOI: https://doi.org/10.1111/medu.12512
Dyrbye L, Thomas M, Shanafelt T. Systematic review of กepression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med 2006; 81: 354-73. DOI: https://doi.org/10.1097/00001888-200604000-00009
Rotenstein L, Ramos M, Torre M, Segal J, Peluso M, Guille C et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students. JAMA 2016; 316: 2214. DOI: https://doi.org/10.1001/jama.2016.17324
Monfared A, Akhondzadeh L, Soleimani R, Maroufizadeh S, Pouy S, Asgari F. Psychological distress and coping strategies among clinicians and medical students during the COVID-19 Pandemic: A cross-sectional study in Guilan, Iran. Shiraz E-Med J 2021; 22: 228-35 DOI: https://doi.org/10.5812/semj.109764
Al-Balas M, Al-Balas H, Jaber H, Obeidat K, Al-Balas H, Aborajooh E et al. Correction to Distance learning in clinical medical education amid COVID-19 pandemic in Jordan: current situation, challenges, and perspectives. BMC Med Ed 2020; 20: 1-7. DOI: https://doi.org/10.1186/s12909-020-02428-3
Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res 2020; 287: 112934: 1-5. DOI: https://doi.org/10.1016/j.psychres.2020.112934
Ahmed N, Khan A, Naveed HA, Moizuddin SM, Khan J. Concerns of undergraduate medical students towards an outbreak of COVID-19. Inter J Cur Med Pharm Res 2020; 6: 5055–62.
Choi B, Jegatheeswaran L, Minocha A, Alhilani M, Nakhoul M, Mutengesa E. The impact of the COVID-19 pandemic on final year medical students in the United Kingdom: a national survey. BMC Medical Ed 2020; 20: 1–11. DOI: https://doi.org/10.1186/s12909-020-02117-1
Lyons, Z., Wilcox, H., Leung, L. and Dearsley, O., 2020. COVID-19 and the mental well-being of Australian medical students: impact, concerns and coping strategies used. Australas Psychiatry 2020; 28: 649-52. DOI: https://doi.org/10.1177/1039856220947945
Turakitwanakan V. Mental health of Srinakharinwirot University medical students. J Psychiatr Assoc Thailand 1997; 42: 88-100.
Kunadison W, Pitanupong J. Mental health and associated factors in Prince of Songkla University medical students. Songkla Med J 2010; 28: 139-44.
Suritikamol L, Hirunviwatgul N, Ratanawilai A. Prevalence and source of stress among the medical cadets and the medical students in Phramongkutklao College of Medicine. J Psychiatr Assoc Thailand 2010; 55: 329-36.
Fear of illness and virus evaluation (FIVE) scales for child-, parent- and adult-report. | Anxiety and Depression Association of America, ADAA [Internet]. Adaa.org. 2021 [cited 25 August 2021]. Available from: https://adaa.org/node/5168
Çölkesen F, Kılınçel O, Sözen M, Yıldız E, Beyaz Ş, Çölkesen F et al. The Impact of SARS-CoV-2 Transmission fear and the COVID-19 pandemic on the mental health of patients with primary immunodeficiency disorders and severe asthma, and other high-risk groups. Asthma Allergy Immunol 2021; 19: 84-91 DOI: https://doi.org/10.21911/aai.651
Oei T, Sawang S, Goh Y, Mukhtar F. Using the Depression Anxiety Stress Scale 21 (DASS-21) across cultures. Int J Psychol 2013;48: 1018-1029. DOI: https://doi.org/10.1080/00207594.2012.755535
Saraswathi I, Saikarthik J, Senthil Kumar K, Madhan Srinivasan K, Ardhanaari M, Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. Peer J 2020; 8: e10164. DOI: https://doi.org/10.7717/peerj.10164
Nakhostin-Ansari A, Sherafati A, Aghajani F, Khonji M, Aghajani R, Shahmansouri N. Depression and anxiety among Iranian medical students during COVID-19 pandemic. Iran J Psychiatry 2020; 15: 228-35. DOI: https://doi.org/10.18502/ijps.v15i3.3815
Torun F, Torun S. The psychological impact of the COVID-19 pandemic on medical students in Turkey. Pak J Med Sci 2020; 36:1355-59 DOI: https://doi.org/10.12669/pjms.36.6.2985
Koh D, Lim M, Chia S, Ko S, Qian F, Ng V, et al. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore. Med Care 2005; 43: 676-82. DOI: https://doi.org/10.1097/01.mlr.0000167181.36730.cc
Nguyen H, Do B, Pham K, Kim G, Dam H, Nguyen T, et al. Fear of COVID-19 scale-associations of its scores with health literacy and health-related behaviors among medical students. Int J Environ Res Public Health 2020; 17: 4164. DOI: https://doi.org/10.3390/ijerph17114164
Van der Merwe L, Botha A, Joubert G. Resilience and coping strategies of undergraduate medical students at the University of the Free State. S Afr J Psychiatr 2020; 26: 1-8. DOI: https://doi.org/10.4102/sajpsychiatry.v26i0.1471
Alsoufi A, Alsuyihili A, Msherghi A, Elhadi A, Atiyah H, Ashini A, et al. Impact of the COVID-19 pandemic on medical education: medical students’ knowledge, attitudes, and practices regarding electronic learning. PLOS ONE 2020; 15: e0242905. DOI: https://doi.org/10.1371/journal.pone.0242905
Ketumarn P, Sitdhiraksa N, Sittironnarit G, Limsricharoen K, Pukrittayakamee P, Wannarit K. Psychiatric disorders and personality problems in medical students at Faculty of Medicine, Siriraj Hospital, Years 1982-2007. J Psychiatr Assoc Thailand 2013; 57: 427-38.
Suritikamol L, Ratanawilai A, Hirunviwatgul N. Prevalence and source of stress among the medical cadets and the medical students in Phramongkutklao College of Medicine. J Psychiatr Assoc Thailand. 2010; 55: 329-36.
Perz C, Lang B, Harrington R. Validation of the fear of COVID-19 scale in a US college sample. Int J Ment Health Addict 2020; 20: 273-83. DOI: https://doi.org/10.1007/s11469-020-00356-3
Xie J, Li X, Luo H, He L, Bai Y, Zheng F, et al. Depressive symptoms, sleep quality and diet during the 2019 novel coronavirus epidemic in China: a survey of medical students. Front Public Health 2021; 8:588578. DOI: https://doi.org/10.3389/fpubh.2020.588578
da Silva F, Neto M. Psychiatric symptomatology associated with depression, anxiety, distress, and insomnia in health professionals working in patients affected by COVID-19: a systematic review with meta-analysis. Prog Neuro-Psychopharmacol Biol Psychiatry 2021; 104: 110057. DOI: https://doi.org/10.1016/j.pnpbp.2020.110057
Yassin A, Al-Mistarehi A, Beni Yonis O, Aleshawi A, Momany S, Khassawneh B. Prevalence of sleep disorders among medical students and their association with poor academic performance: a cross-sectional study. Ann Med Surg 2020; 58: 124-29. DOI: https://doi.org/10.1016/j.amsu.2020.08.046
Romo-Nava, F, Tafoya, S, Gutiérrez-Soriano, J, Osorio, Y, Carriedo, P, Ocampo, B, et al. The association between chronotype and perceived academic stress to depression in medical students. Chronobiol Int 2016; 33: 1359-68. DOI: https://doi.org/10.1080/07420528.2016.1217230
Adrien J. Neurobiological bases for the relation between sleep and depression. Sleep Med Rev 2002; 6: 341-51. DOI: https://doi.org/10.1053/smrv.2001.0200
Kongsomboon K. Academic achievement correlated to stress, depression, and sleep deprivation in medical students. Srinagarind Med J 2013: 25: 109-14.
Xiang Y, Yang Y, Li W, Zhang L, Zhang Q, Cheung T et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020; 7: 228-29. DOI: https://doi.org/10.1016/S2215-0366(20)30046-8
Mittal R, Su L, Jain R. COVID-19 mental health consequences on medical students worldwide. J Community Hosp Intern Med Perspect 2021; 11: 296-8. DOI: https://doi.org/10.1080/20009666.2021.1918475
Coyle C, Ghazi H, Georgiou I. The mental health and well-being benefits of exercise during the COVID-19 pandemic: a cross-sectional study of medical students and newly qualified doctors in the UK. Ir J Med Sci 2020; 190: 925-6. DOI: https://doi.org/10.1007/s11845-020-02423-z
Aardal-Eriksson E, Eriksson T, Holm A, Lundin T. Salivary cortisol and serum prolactin in relation to stress rating scales in a group of rescue workers. Biol Psychiatry 1999; 46: 850-55. DOI: https://doi.org/10.1016/S0006-3223(98)00381-3
Rai B, Kaur J, Foing B. Salivary amylase and stress during stressful environment: Three Mars analog mission crews study. Neurosci Lett 2012; 518: 23-6. DOI: https://doi.org/10.1016/j.neulet.2012.04.034
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.