CANCER RATIO-BASED DIAGNOSTIC TOOL IN IDENTIFYING MALIGNANT PLEURAL EFFUSION: SENSITIVITY, SPECIFICITY AND CLINICAL INSIGHTS
DOI:
https://doi.org/10.55374/jseamed.v7.177Keywords:
cancer ratio, malignant pleural effusion, exudative, lymphocytic, pleural effusionAbstract
Background: Malignant pleural effusion (MPE) is a common cause of exudative lymphocytic pleural effusion. Although pleural fluid evaluation is routinely performed, cytology or histopathology remains the gold standard for MPE diagnosis. The cancer ratio (CR), calculated by comparing serum LDH to pleural fluid ADA levels, has shown promise in diagnosing MPE. However, no studies have investigated its utility in the Thai population, which has a high tuberculosis prevalence.
Objectives: This study aimed to evaluate the diagnostic accuracy of the CR in MPE diagnosis, compare clinical and pleural fluid parameters between MPE and nonMPE cases, determine the appropriate CR cut-off for the Thai population and develop a prediction score for prediagnosing MPE.
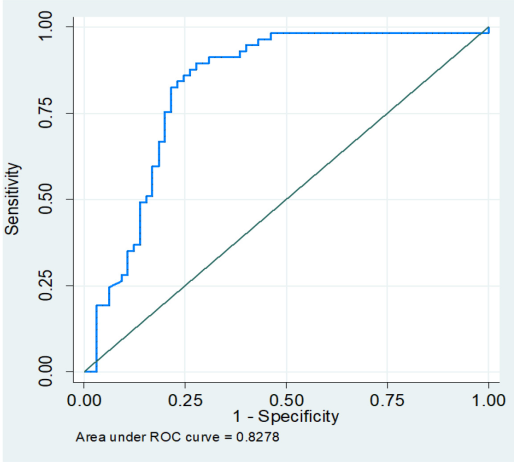
Results: Between July 2021 and December 2022, patients presenting exudative lymphocytic pleural effusion were included in the study. Demographics, symptoms, radiographic findings and pleural fluid parameters were collected and cytology/histopathology served as the reference test. CR performance was assessed using receiver operating characteristic curves, and a prediction score was developed using multivariable logistic regression analysis. Among 122 patients, 46.7% received a diagnosis of MPE. The CR exhibited a sensitivity of 87.7% and specificity of 72.3% (AUC 0.83) with a cut-off level >10. Patients with MPE showed longer symptom duration, lower fever and massive pleural effusion, which were more common in MPE than nonMPE cases. A prediction score incorporating symptom duration, fever history, effusion amount and CR demonstrated superior diagnostic performance for MPE (AUC 0.94) compared with the CR alone.
Conclusion: The CR can effectively differentiate MPE from nonMPE among patients with exudative lymphocytic pleural effusion. A cut-off level >10 is recommended for diagnosing MPE in the Thai population. Combining clinical, radiologic and CR data may aid in prediagnosing MPE; however, further research is needed for validation.
Downloads
Metrics
References
Pettersson T, Riska H. Diagnostic value of total and differential leukocyte counts in pleural effusions. Acta Med Scand 1981; 210: 129-35. DOI: https://doi.org/10.1111/j.0954-6820.1981.tb09788.x
Davies HE, Davies RJ, Davies CW, Group BTSPDG. Management of pleural infection in adults: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010; 65 Suppl 2: ii41-53. DOI: https://doi.org/10.1136/thx.2010.137000
Saiphoklang N, Kanitsap A, Ruchiwit P. Diagnostic Value of Pleural Fluid Adenosine Deaminase in Tuberculous Pleuritis at Thammasat University Hospital. J Med Assoc Thai 2016; 99 Suppl 4: S1-9.
Aggarwal AN, Agarwal R, Sehgal IS, Dhooria S. Adenosine deaminase for diagnosis of tuberculous pleural effusion: A systematic review and meta-analysis. PLoS One 2019; 14: e0213728. DOI: https://doi.org/10.1371/journal.pone.0213728
Liang QL, Shi HZ, Wang K, Qin SM, Qin XJ. Diagnostic accuracy of adenosine deaminase in tuberculous pleurisy: a meta-analysis. Respir Med 2008; 102: 744-54. DOI: https://doi.org/10.1016/j.rmed.2007.12.007
Kaul V, McCracken DJ, Rahman NM, Epelbaum O. Contemporary Approach to the Diagnosis of Malignant Pleural Effusion. Ann Am Thorac Soc 2019; 16: 1099-106. DOI: https://doi.org/10.1513/AnnalsATS.201902-189CME
Metintas M, Ak G, Dundar E, Yildirim H, Ozkan R, Kurt E, et al. Medical thoracoscopy vs CT scan-guided Abrams pleural needle biopsy for diagnosis of patients with pleural effusions: a randomized, controlled trial. Chest 2010; 137: 1362-8. DOI: https://doi.org/10.1378/chest.09-0884
Dixon G, de Fonseka D, Maskell N. Pleural controversies: image guided biopsy vs. thoracoscopy for undiagnosed pleural effusions? J Thorac Dis 2015; 7: 1041-51.
Liang QL, Shi HZ, Qin XJ, Liang XD, Jiang J, Yang HB. Diagnostic accuracy of tumour markers for malignant pleural effusion: a meta-analysis. Thorax 2008; 63: 35-41. DOI: https://doi.org/10.1136/thx.2007.077958
Antonangelo L, Sales RK, Cora AP, Acencio MM, Teixeira LR, Vargas FS. Pleural fluid tumour markers in malignant pleural effusion with inconclusive cytologic results. Curr Oncol 2015; 22: e336-41. DOI: https://doi.org/10.3747/co.22.2563
Verma A, Abisheganaden J, Light RW. Identifying Malignant Pleural Effusion by A Cancer Ratio (Serum LDH: Pleural Fluid ADA Ratio). Lung 2016; 194: 147-53. DOI: https://doi.org/10.1007/s00408-015-9831-6
Asciak R, Rahman NM. Malignant Pleural Effusion: From Diagnostics to Therapeutics. Clin Chest Med 2018; 39: 181-93. DOI: https://doi.org/10.1016/j.ccm.2017.11.004
Han YQ, Zhang L, Yan L, Ouyang PH, Li P, Hu ZD. Diagnostic accuracy of cancer ratio for malignant pleural effusion: a systematic review and meta-analysis. Ann Transl Med 2019; 7:5 54. DOI: https://doi.org/10.21037/atm.2019.09.85
Kremer R, Best LA, Savulescu D, Gavish M, Nagler RM. Pleural fluid analysis of lung cancer vs benign inflammatory disease patients. Br J Cancer 2010; 102: 1180-4. DOI: https://doi.org/10.1038/sj.bjc.6605607
Gottehrer A, Taryle DA, Reed CE, Sahn SA. Pleural fluid analysis in malignant mesothelioma. Prognostic implications. Chest 1991; 100: 1003-6. DOI: https://doi.org/10.1378/chest.100.4.1003
Saiphoklang N, Kanitsap A, Nambunchu A. Differences in clinical manifestations and pleural fluid characteristics between tuberculous and malignant pleural effusions. Southeast Asian J Trop Med Public Health 2015; 46: 496-503.
Zhang F, Hu L, Wang J, Chen J, Chen J, Wang Y. Clinical value of jointly detection serum lactate dehydrogenase/pleural fluid adenosine deaminase and pleural fluid carcinoembryonic antigen in the identification of malignant pleural effusion. J Clin Lab Anal 2017; 31: e22106. DOI: https://doi.org/10.1002/jcla.22106
Zhang Y, Li X, Liu J, Hu X, Wan C, Zhang R, et al. Diagnostic accuracy of the cancer ratio for the prediction of malignant pleural effusion: evidence from a validation study and meta-analysis. Ann Med 2021; 53: 558-66. DOI: https://doi.org/10.1080/07853890.2021.1906943
Valdes L, San-Jose E, Ferreiro L, Gonzalez-Barcala FJ, Golpe A, Alvarez-Dobano JM, et al. Combining clinical and analytical parameters improves prediction of malignant pleural effusion. Lung 2013; 191: 633-43. DOI: https://doi.org/10.1007/s00408-013-9512-2
Pan Y, Bai W, Chen J, Mao Y, Qian X, Xu K, et al. Diagnosing malignant pleural effusion using clinical and analytical parameters. J Clin Lab Anal 2019; 33: e22689. DOI: https://doi.org/10.1002/jcla.22689
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.