APPLICATION OF ARTIFICIAL INTELLIGENCE TO ASSIST HIP FRACTURE DIAGNOSIS USING PLAIN RADIOGRAPHS
DOI:
https://doi.org/10.55374/jseamed.v6i0.111Keywords:
Artificial intelligence, Hip fractureAbstract
Background: Most hip fractures occur among elderly people. They are usually treated in the emergency room where orthopedic surgeons may not be readily available. The problem of delayed diagnosis and treatment results increase risks of further complications and mortality rate. Thus, applying artificial intelligence (AI) can assist physicians having limited experience to rapidly and confidently diagnose hip fractures using radiographs.
Objective: This study aimed to validate AI programs to assist diagnosing of hip fractures on plain radiographs.
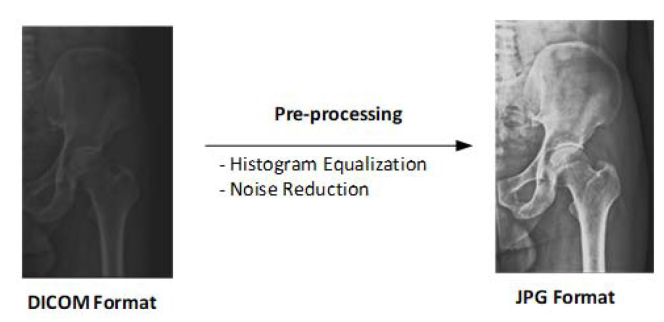
Methods: This study employed a retrospective diagnostic study design. From 1 January 2015 to 31 December 2019, compiled ortho pelvis, anterior-posterior (AP) films from the diagnosis of hip fractures at Ananthamahidol Hospital were performed. The performance of the AI program was compared with one orthopedic surgeon who reviewed the same images. The accuracy, sensitivity and specificity of the diagnosis of hip fractures between the orthopedic surgeon and AI program were analyzed.
Results: In total, 217 patients were enrolled in this study. Of these, 56 (28.5%) were male and 161 (74.2%) female. Areas of hip fractures were as follow: intertrochanteric (108, 49.8%), femoral neck (102, 47.0%), subtrochanteric (6, 2.7%) and femoral head (1, 0.5%). The orthopedic surgeon and AI program revealed an accuracy of 93.59% (95%CI 90.8-95.73) vs. 81.24% (95% CI 77.17-84.85), sensitivity of 90.30% (95% CI 85.60-93.90) vs. 89.40% (95%CI 84.50-93.20) and specificity of 97.10% (95%CI 93.60-98.90) vs. 72.5% (95%CI 65.90-78.50), respectively.
Conclusion: Our results showed that the AI model (VGG16) showed a sensitivity of 89.40% vs. 90.30% obtained from the orthopedic surgeon. Thus, improvement in the sensitivity and specificity of AI software is further required. In the future, AI models have the potential as useful tools for emergent screening and evaluation of patients with hip fractures using plain radiographs, especially in the Emergency Department where orthopedic surgeons may not be readily available.
Downloads
Metrics
References
Johnell O, Kanis JA. An estimate of worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 2006; 17: 1726-33. DOI: https://doi.org/10.1007/s00198-006-0172-4
Gullberg B, Johnell O, Kanis JA. Worldwide projections for hip fracture. Osteoporos Int 1977; 7: 407-13. DOI: https://doi.org/10.1007/PL00004148
Guzon-lllecas O, Fernandez EP, Villarias NC, Donate FJQ, Pena M, Alonso-Blas C, et al. Mortality after osteoporotic hip fracture: incidence, trends and associated factors. J. Orthop Surg Res 2019; 14: 1-9. DOI: https://doi.org/10.1186/s13018-019-1226-6
CL Daugaard, HL Jorgensen, T Riis, JB Lauritzen, BR Duss, SVD Mark. Is mortality after hip fracture associated with surgical delay or admission during weekend and public holidays? Acta Orthop 2012; 83: 609-13. DOI: https://doi.org/10.3109/17453674.2012.747926
Ricci G, Longaray MP, Goncalves RZ, Neto ASU, Manente M, Barbosa LBH. Evaluation of the mortality rate one year after hip fracture and factors relating to diminished survival among elderly people. Rev Bras Orthop 2012; 47: 304-09. DOI: https://doi.org/10.1016/S2255-4971(15)30103-8
Downey C, Kelly M, Quinland JF. Changing trends in the mortality rate at 1-year post hip fracture-a systematic review. World J Orthop 2019; 10: 166-75. DOI: https://doi.org/10.5312/wjo.v10.i3.166
Cui Z, Feng H, Meng X, Zhuang S, Liu Z, Ye K, et al. Age-specific 1-year mortality rate after hip fracture based on populations in mainland China between the year 2000 and 2018. Arch Osteoporos 2019; 14: 1-10. DOI: https://doi.org/10.1007/s11657-019-0604-3
Chow SKH, Qin JH, Wong RMY, Yuen WF, Ngai WK, Tang N, et al. One year mortality in displaced intracapsular hip fracture and associated risk: a report of Chinese-based fragility fracture registry. J Orthop Surg Res 2018; 13: 1-6 DOI: https://doi.org/10.1186/s13018-018-0936-5
Seung-Ju Kim, Hyundai-Soo Park, Dong-Woo Lee. Outcome of nonoperative treatment for hip fractures in elderly patients: A systematic review of recent literature. J Orthop Surg 2020; 28: 1-8 DOI: https://doi.org/10.1177/2309499020936848
Moran CG, Wenn RT, Taylor AM, Sikand M. Early mortality after hip fracture: is delay before surgery important? JBJS Am 2005; 87: 483-89 DOI: https://doi.org/10.2106/JBJS.D.01796
Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systemic review, meta-analysts and meta-regression. Can J Anesth 2008; 55: 146-54. DOI: https://doi.org/10.1007/BF03016088
Klestil T, Roder C, Stotter C, Winkler B, Nehrer S, Lutz, M, et al. Impact of timing of surgery in elderly hip fracture patients: a systematic review and meta-analysis. Sci Rep 2018; 8: 1-15 DOI: https://doi.org/10.1038/s41598-018-32098-7
Sobolev B, Guy P, Sheehan KJ, Kuramoto L, Sutherland JM, Levy AR, et al. Mortality effects of timing alternative for hip fracture surgery. CMAJ 2018; 190: 923-32. DOI: https://doi.org/10.1503/cmaj.171512
Matisson L, Bojan A, Enocson A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fracture:data from the Swedish fracture register. BMC Muscoskel Disord 2018; 19: 1-8. DOI: https://doi.org/10.1186/s12891-018-2276-3
Sa-Ngasoonsong, Kulachote N, Sirisreetreerax N, Chanplakorn P, Laohajaroensombat S, Seeraprom J, et al. Outcome of early hip fracture surgery in elderly patients in Ramathipbodi Hospital. Rama Med J 2013;36: 3-12.
MW Kirby, C Spritzer. Radiographic detection of hip and pelvic fractures in the Emergency Department. AJR Am J Roentgenol 2010; 194: 1054-60. DOI: https://doi.org/10.2214/AJR.09.3295
Dominquez S, Lui P, Roberts C, Mendell M, Richman PB. Prevalence of traumatic hip and pelvic fractures in patients with suspected hip fracture and negative initial standard radiographs. Acad Emerg Med 2005; 12: 366-70. DOI: https://doi.org/10.1111/j.1553-2712.2005.tb01959.x
Je S, Kim H, Ryu S, Cho S, Oh S, Kang T, et al. The consequence of delayed diagnosis of occult hip fracture. J Trauma Inj 2015; 28: 91-97. DOI: https://doi.org/10.20408/jti.2015.28.3.91
Sodozai Z, Davies R, Warner J. The sensitivity of CT scan in diagnosis occult femoral neck fractures. Injury Int J 2016; 47: 2769-71. DOI: https://doi.org/10.1016/j.injury.2016.10.019
Yun BJ, Hunink M, Prabhakar AM, Heng M, Lui SW, Qudsi R, et al. Diagnosis imaging stratigies for occult hip fractures. Acad Emerg Med 2016; 23: 1161-69. DOI: https://doi.org/10.1111/acem.13026
Raval P, Mayne AIW, PM Yeap, Oliver TB, Jirawala A, Sripada S. Outcome of MRI detected occult neck of femur fracture: Do they represent a less severe injury with improved outcomes? Hip Pelvis 2019; 31: 18-22. DOI: https://doi.org/10.5371/hp.2019.31.1.18
Foex BA, Russell A. CT versus MRI for occult hip fracture. Emerg Med J 2018; 35: 645-47. DOI: https://doi.org/10.1136/emermed-2018-208093.3
Trenton T. Kellock, Bharti Khurana, Jacob C. Mandell. Diagnostic performance of CT for occult proximal femoral fractures. A systematic review and meta-analysis. AJR Am J Roentgenol 2019; 213: 1324-30. DOI: https://doi.org/10.2214/AJR.19.21510
Urakawa T, Tanaka Y, Goto S, Matsuzawa H, Watanabe K, Endo N. Detecting intertrochanteric hip fracture with orthopedist level accuracy using a deep convolutional neural network. Skeletal Radiol 2019; 48: 239-44. DOI: https://doi.org/10.1007/s00256-018-3016-3
CT Cheng, TY Ho, TY Lee, CC Chang, CC Chou, CC Chen, et al. Application of a deep learning algorithm for detecting and visualization of hip fracture on plain radiographs. Eur Radiol 2019; 29: 5469-77. DOI: https://doi.org/10.1007/s00330-019-06167-y
Adams M, Chen W, Holcdorf D, McCusker MW, Howe PDL, Gaillard F. Deep learning versus perceptual training for the detection of neck of femur fracture. J Med Imaging Radiat Oncol 2019; 63: 27-32. DOI: https://doi.org/10.1111/1754-9485.12828
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.