ASSOCIATION WITH INCIDENCE OF ISCHEMIC HEART DISEASE BASED ON THE ESTIMATED GLOMERULAR FILTRATION RATE IN THE POPULATION OF THE THREE SOUTHERN BORDER PROVINCES OF THAILAND
DOI:
https://doi.org/10.55374/jseamed.v9.242Keywords:
estimated glomerular filtration rate (eGFR), ischemic heart disease (IHD), chronic kidney disease (CKD), cardiovascular risk, retrospective cohort studyAbstract
Background: Declining kidney function, as reflected by a reduced estimated glomerular filtration rate (eGFR), has been associated with an increased risk of ischemic heart disease (IHD). However, limited evidence is available in the population residing in Thailand’s three southern border provinces. Objective: This study aimed to examine the association between estimated eGFR and the incidence of IHD in the population of Thailand’s three southern border provinces.
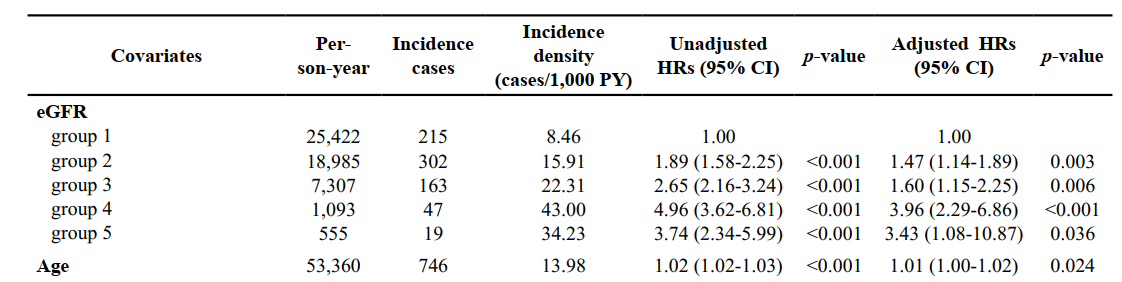
Methods: A retrospective cohort study was conducted using electronic medical records from three government hospitals between October 1, 2018, and September 30, 2023. Adults aged 30 years or older with baseline eGFR data were categorized into five groups based on their eGFR levels. The outcome was incident IHD, identified using ICD-10 codes. Cox proportional hazards regression was used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs), adjusting for relevant covariates.
Results: Among 16,763 participants followed for a total of 53,360 person-years, 746 developed IHD. The cumulative incidence was 4.5% (95% CI: 4.0–5.0%), and the incidence density was 13.98 cases per 1,000 person-years. A significant inverse relationship was observed between eGFR and IHD incidence (p < 0.001). Compared with participants with eGFR ≥90.00 mL/min/1.73 m², the adjusted HRs for IHD were 1.89 (95% CI: 1.58-2.25) for eGFR 60.00-89.99, 2.65 (95% CI: 2.16-3.24) for 30.00–59.99, 4.96 (95% CI: 3.62-6.81) for 15.00-29.99, and 3.74 (95% CI: 2.34-5.99) for <15.00 mL/min/1.73 m². A graded increase in IHD risk was observed across lower eGFR groups. Other significant risk factors included older age, sex, higher systolic blood pressure, and atrial fibrillation, while higher high-density lipoprotein cholesterol (HDL-C) levels were associated with a reduced risk of IHD.
Conclusion: Reduced eGFR was independently associated with a higher risk of IHD, even among individuals with mildly impaired kidney function. These findings support the potential role of eGFR in cardiovascular risk assessment and the development of targeted prevention strategies in high-risk populations.
Downloads
Metrics
References
Elliott M. Antman, Joseph Loscalzo. Ischemic Heart Disease. In: Joseph Loscalzo, Dennis L. Kasper, Dan L. Longo, Anthony S. Fauci, Stephen L. Hauser, J. Larry Jameson, editors. Harrison's Principles of Internal Medicine, 21St Ed. McGraw-Hill LLC.; 2022. p. 7481-536.
Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, et al. Heart disease and stroke statistics-2023 Update: A report from the American Heart Association. Circulation 2023; 147(8). DOI: https://doi.org/10.1161/CIR.0000000000001137 DOI: https://doi.org/10.1161/CIR.0000000000001137
World Health Organization. The top 10 causes of death. WHO's Global Health Estimates. 2020 [cited 2024 February 19]. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
Scholes S, Mindell JS. Health survey for England 2017 Cardiovascular diseases [Internet]. 2018 [cited 2024 May 16]. Available from: https://www.statisticsauthority.gov.uk/assessment/code-of-practice
HU SS. Report on cardiovascular health and diseases in China 2021: an updated summary. J Geriatr Cardiol 2023; 20: 399–430. Available from: https://www.sciopen.com/article/0.26599/1671-5411.2023.06.001 DOI: https://doi.org/10.26599/1671-5411.2023.06.001 DOI: https://doi.org/10.26599/1671-5411.2023.06.001
Division of Non-Communicable Diseases. Number and mortality rate from 5 non-communicable diseases, 2017-2021 [Internet]. Nonthaburi; 2023 Jan [cited 2023 December 10]. Available from: http://www.thaincd.com/2016/mission3
Sakboonyarat B, Rangsin R. Hospital admission and mortality rates for ischemic heart disease in Thailand: 2012-2021. BMC Res Notes 2024; 17:142. DOI: https://doi.org/10.1186/s13104-024-06803-x DOI: https://doi.org/10.1186/s13104-024-06803-x
AKF's Medical Advisory Committee. Blood test: eGFR (estimated glomerular filtration rate) [Internet]. American Kidney Fund, FIGHTING ON ALL FRONTS. 2023 [cited 2024 March 16]. Available from: https://www.kidneyfund.org/all-about-kidneys/tests/blood-test-egfr
Chronic Kidney Disease Prognosis Consortium, Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 2010; 375: 375: 2073-81. DOI: https://doi.org/10.1016/S0140-6736(10)60674-5 DOI: https://doi.org/10.1016/S0140-6736(10)60674-5
Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, et al. The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int 2011; 80:17-28. DOI: https://doi.org/10.1038/ki.2010.483 DOI: https://doi.org/10.1038/ki.2010.483
van der Velde M, Matsushita K, Coresh J, Astor BC, Woodward M, Levey AS, et al. Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality. A collaborative meta-analysis of high-risk population cohorts. Kidney Int 2011; 79: 1341-52. DOI: https://doi.org/10.1038/ki.2010.536 DOI: https://doi.org/10.1038/ki.2010.536
Jin B, Bai X, Han L, Liu J, Zhang W, Chen X. Association between kidney function and Framingham Global Cardiovascular Disease risk score: A Chinese longitudinal study. PLoS One 2014; 9: e86082. DOI: https://doi.org/10.1371/journal.pone.0086082 DOI: https://doi.org/10.1371/journal.pone.0086082
Widhi Nugroho A, Arima H, Miyazawa I, Fujii T, Miyamatsu N, Sugimoto Y, et al. The association between glomerular filtration rate estimated on admission and acute stroke outcome: The Shiga Stroke Registry. J Atheroscler Thromb 2018 ; 25: 570-9. DOI: https://doi.org/10.5551/jat.42812
Zhang L, Zuo L, Wang F, Wang M, Wang S, Lv J, et al. Cardiovascular disease in early stages of chronic kidney disease in a Chinese population. J Am Soc Nephrol 2006; 17: 2617-21. Available from: https://journals.lww.com/00001751-200609000-00034. DOI: https://doi.org/10.1681/ASN.2006040402
Park SK, Kim MH, Ha E, Jung JY, Oh CM, Choi JM, et al. The risk for incident ischemic heart disease according to estimated glomerular filtration rate in A Korean population. J Atheroscler Throm 2020; 27: 461-70. DOI: https://doi.org/10.5551/jat.50757 DOI: https://doi.org/10.5551/jat.50757
Ichii T, Morimoto R, Okumura T, Ishii H, Tatami Y, Yamamoto D, et al. Impact of renal functional/morphological dynamics on the calcification of coronary and abdominal arteries in patients with chronic kidney disease. J Atheroscler Thromb 2017; 24: 1092-104. DOI: https://doi.org/10.5551/jat.39271 DOI: https://doi.org/10.5551/jat.39271
Sibilitz KL, Benn M, Nordestgaard BG. Creatinine, eGFR and association with myocardial infarction, ischemic heart disease and early death in the general population. Atherosclerosis 2014; 237: 67-75. DOI: https://doi.org/10.1016/j.atherosclerosis.2014.08.040 DOI: https://doi.org/10.1016/j.atherosclerosis.2014.08.040
Widhi Nugroho A, Arima H, Miyazawa I, Fujii T, Miyamatsu N, Sugimoto Y, et al. The association between glomerular filtration rate estimated on admission and acute stroke outcome: The Shiga Stroke Registry. J Atheroscler Thromb 2018; 25: 570-9. DOI: https://doi.org/10.5551/jat.42812 DOI: https://doi.org/10.5551/jat.42812
Zhang L, Zuo L, Wang F, Wang M, Wang S, Lv J, et al. Cardiovascular disease in early stages of chronic kidney disease in a Chinese population. J Am Soc Nephrol 2006; 17: 2617-21. DOI: https://doi.org/10.1681/ASN.2006040402 DOI: https://doi.org/10.1681/ASN.2006040402
Shimbo Y, Suzuki S, Ishii H, Shibata Y, Tatami Y, Harata S, et al. Association of estimated glomerular filtration rate and proteinuria with lipid-rich plaque in coronary artery disease. Circ J 2015; 79: 2263-70. DOI: https://doi.org/10.1253/circj.CJ-15-0460 DOI: https://doi.org/10.1253/circj.CJ-15-0460
Health Data Center (HDC). Report on health indicators at the Ministry of Public Health Level, Thailand, 2021. https://hdcservice.moph.go.th/hdc/reports/report_kpi.php?-flag_kpi_level=1&flag_kpi_year=2022&source=pformated/format1.php&id=d-843f25a088253c22344d771113cf409#.2021.
Inker LA, Eneanya ND, Coresh J, Tighiouart H, Wang D, Sang Y, et al. New creatinineand cystatin C–based equations to estimate GFR without Race. N Engl J Med 2021; 385:1737-49. DOI: https://doi.org/10.1056/NEJMoa2102953 DOI: https://doi.org/10.1056/NEJMoa2102953
Bureau of Policy and Strategy of the PSM of PH. CHAPTER IX Diseases of the circulatory system (I10-I99). In: Kanthee Sangkhawasi, Wittaya Sreedama, Wassa Paoin, Maliwan Yuenyongsuwan, Jindarat Khumdet, Jiraporn Sumtip, editors. International Statistical Classification of Diseases and Related Health Problems, 10th Revision, Thai Modification (ICD-10-TM). Bureau of Policy and Strategy, Office of the Permanent Secretary, Ministry of Public Health; 2012. p. 284-7
Dube P, DeRiso A, Patel M, Battepati D, Khatib-Shahidi B, Sharma H, et al. Vascular calcification in chronic kidney disease: diversity in the vessel wall. Biomedicines 2021; 9: 404. DOI: https://doi.org/10.3390/biomedicines9040404 DOI: https://doi.org/10.3390/biomedicines9040404
Ekici B. Effects of glomerular filtration rate on the severity of coronary heart disease. Turk Kardiyol Dern 2016; 44: 123-9. DOI: https://doi.org/10.5543/tkda.2015.48323 DOI: https://doi.org/10.5543/tkda.2015.48323
Ninomiya T, Kiyohara Y, Kubo M, Tanizaki Y, Doi Y, Okubo K, et al. Chronic kidney disease and cardiovascular disease in a general Japanese population: The Hisayama Study. Kidney Int 2005; 68: 228-36. DOI: https://doi.org/10.1111/j.1523-1755.2005.00397.x DOI: https://doi.org/10.1111/j.1523-1755.2005.00397.x
Weiner DE, Tabatabai S, Tighiouart H, Elsayed E, Bansal N, Griffith J, et al. Cardiovascular outcomes and all-cause mortality: exploring the interaction between CKD and cardiovascular disease. Am J Kidney Dis 2006; 48: 392-401. DOI: https://doi.org/10.1053/j.ajkd.2006.05.021 DOI: https://doi.org/10.1053/j.ajkd.2006.05.021
Groenewegen A, Zwartkruis VW, Smit LJ, de Boer RA, Rienstra M, Hoes AW, et al. Sex-specific and age-specific incidence of ischaemic heart disease, atrial fibrillation and heart failure in community patients with chronic obstructive pulmonary disease. BMJ Open Respir Res 2022; 9: e001307. DOI: https://doi.org/10.1136/bmjresp-2022-001307 DOI: https://doi.org/10.1136/bmjresp-2022-001307
Sakboonyarat B, Rangsin R. Prevalence and associated factors of ischemic heart disease (IHD) among patients with diabetes mellitus: a nation-wide, cross-sectional survey. BMC Cardiovasc Disord 2018; 18:151. DOI: https://doi.org/10.1186/s12872-018-0887-0 DOI: https://doi.org/10.1186/s12872-018-0887-0
Azab M, Al-Shudifat AE, Johannessen A, Al-Shdaifat A, Agraib LM, Tayyem RF. Are risk factors for coronary artery disease different in persons with and without obesity? Metab Syndr Relat Disord 2018; 16: 440-5. DOI: https://doi.org/10.1089/met.2017.0152 DOI: https://doi.org/10.1089/met.2017.0152
Chuang SY, Chen JH, Yeh WT, Wu CC, Pan WH. Hyperuricemia and increased risk of ischemic heart disease in a large Chinese cohort. Int J Cardiol 2012; 154: 316-21. DOI: https://doi.org/10.1016/j.ijcard.2011.06.055 DOI: https://doi.org/10.1016/j.ijcard.2011.06.055
Muneeb M, Khan AH, Khan Niazi A, Khan MU, Chatha ZJ, Kazmi T, et al. Patterns of dyslipidemia among acute coronary syndrome (ACS) patients at a tertiary care hospital in Lahore, Pakistan. Cureus 2022; 14: e32378. DOI: https://doi.org/10.7759/cureus.32378 DOI: https://doi.org/10.7759/cureus.32378
Razo C, Welgan CA, Johnson CO, McLaughlin SA, Iannucci V, Rodgers A, et al. Effects of elevated systolic blood pressure on ischemic heart disease: a burden of proof study. Nat Med 2022; 28: 2056-65. DOI: https://doi.org/10.1038/s41591-022-01974-1 DOI: https://doi.org/10.1038/s41591-022-01974-1
Kea B, Manning V, Alligood T, Raitt M. A Review of the relationship of atrial fibrillation and acute coronary syndrome. Curr Emerg Hosp Med Rep 2016; 4: 107-18. DOI: https://doi.org/10.1007/s40138-016-0105-2 DOI: https://doi.org/10.1007/s40138-016-0105-2
Barter P, Gotto AM, LaRosa JC, Maroni J, Szarek M, Grundy SM, et al. HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Eng J Med 2007; 357: 1301-10. DOI: https://doi.org/10.1056/NEJMoa064278 DOI: https://doi.org/10.1056/NEJMoa064278
Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function — Measured and estimated glomerular filtration rate. N Eng J Med 2006; 354: 2473-83. DOI: https://doi.org/10.1056/NEJMra054415 DOI: https://doi.org/10.1056/NEJMra054415
Astor BC, Levey AS, Stevens LA, Van Lente F, Selvin E, Coresh J. Method of glomerular filtration rate estimation affects prediction of mortality risk. J Am Soc Nephrol 2009; 20: 2214-22. DOI: https://doi.org/10.1681/ASN.2008090980 DOI: https://doi.org/10.1681/ASN.2008090980
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.