ASSOCIATION OF THE TYPE OF INTRACEREBRAL HEMORRHAGE WITH SERIOUS COMPLICATIONS AND PREDICTIVE FACTORS FOR HEMORRHAGIC TRANSFORMATION AFTER THROMBOLYTIC TREATMENT IN PATIENTS WITH ACUTE ISCHEMIC STROKE
DOI:
https://doi.org/10.55374/jseamed.v8.186Keywords:
Intracerebral hemorrhage, Acute stroke, Thrombolysis, Mortality, ComplicationsAbstract
Background: Accurate classification of postthrombolytic intracerebral hemorrhage (ICH) subtypes is vital for predicting stroke outcomes and managing ICH. Currently, the recommended classification criteria are the European Cooperative Acute Stroke Study III criteria, including two primary categories: hemorrhagic infarction (HI) and parenchymal hematoma (PH).
Objectives: The primary objective of this study was to assess the contribution of various ICH subtypes to serious complications, with the secondary aim to identify associated predictors.
Methods: The study examined medical records of patients with acute ischemic stroke receiving thrombolysis at Saraburi Hospital from 2014 to 2022. The logit model with the margins command assessed the association of ICH subtypes with serious complications, and multinomial logistic regression identified potential predictors for HI and PH.
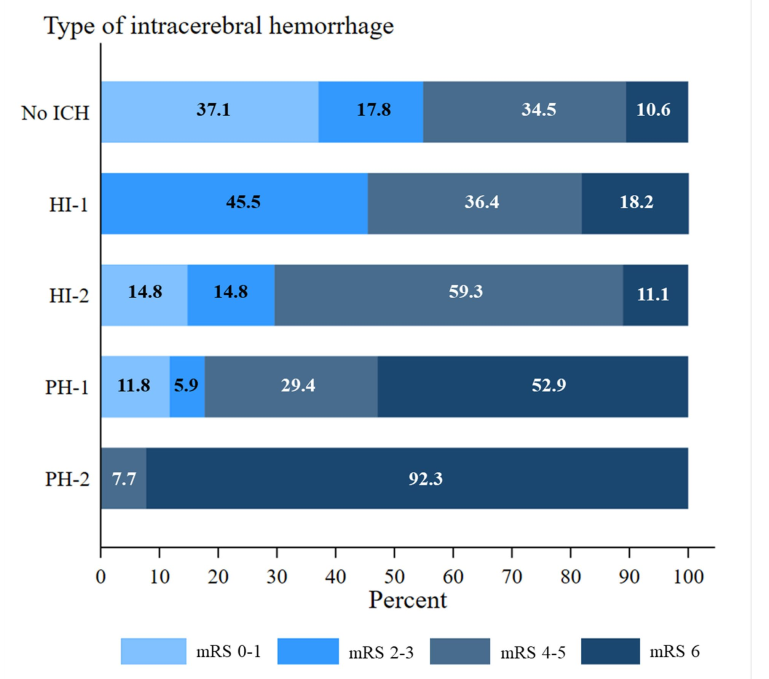
Results: Among 345 patients, HI-1, HI-2, PH-1 and PH-2 had prevalence rates of 3.2, 7.8, 4.9 and 7.5%, respectively, while 76.5% did not have ICH. PH-2 demonstrated the strongest correlation with inhospital mortality (adjusted risk ratio [RR] 2.83, 95% CI 1.56-5.13), invasive mechanical ventilator requirement (adjusted RR 3.93, 95% CI 2.09-7.39) and hematoma evacuation (adjusted RR 4.58, 95% CI 1.17-17.95) compared with patients of non-ICH. HI demonstrated a significant prolongation of hospitalization. (adjusted RR 3.30, 95% CI 1.53-7.12). Multinomial logistic regression analysis revealed that prior use of antiplatelet drugs, antihypertensive treatment before rt-PA, white blood cell count ≥11,750 cells/mm3 and baseline Alberta stroke program early CT scores ≤7 were independent predictors for PH. The adjusted odds ratios were 3.06 (95% CI, 1.23-7.57), 6.95 (95% CI, 2.62-18.45), 6.01 (95% CI, 2.17-16.65) and 5.01 (95% CI, 2.00-12.60), respectively.
Conclusion: The PH-2 subtype was associated with the highest mortality, while our study demonstrated that the HI subtype, previously considered relatively benign with successful early recanalization, showed a significant prolongation of hospitalization compared with that of patients of non-ICH. High-risk patients of ICH require intensive monitoring to reduce complications.
Downloads
Metrics
References
O'carroll CB, Aguilar MI. Management of postthrombolysis hemorrhagic and orolingual angioedema complications. Neurohospitalist 2015; 5: 133-41. https://doi.org/10.1177/1941874415587680
Balami JS, Sutherland BA, Buchan AM. Complications associated with recombinant tissue plasminogen activator therapy for acute ischaemic stroke. CNS Neurol Disord-Drug Targets (Formerly Curr Drug Targets - CNS & Neurod Disord), 2013; 12: 155-69. https://doi.org/10.2174/18715273112119990050
Seet RCS, Rabinstein AA. Symptomatic intracranial hemorrhage following intravenous thrombolysis for acute ischemic stroke: A critical review of case definitions. Cerebrovasc Dis 2012; 34: 106-14. https://doi.org/10.1159/000339675
Choi HY, Cho Y, Kim W, Minn YK, Kang GH, Jang YS, et al. Analysis of mortality in intracerebral hemorrhage patients with hyperacute ischemic stroke treated using thrombolytic therapy: A nationwide population-based cohort study in South Korea. J Pers Med 2022; 12: 1260. https://doi.org/10.3390/jpm12081260
Jensen M, Schlemm E, Cheng B, Lettow I, Quandt F, Boutitie F, et al. Clinical Characteristics and outcome of patients with hemorrhagic transformation after intravenous thrombolysis in the WAKE-UP trial. Front Neurol 2020; 11: 1-8. https://doi.org/10.3389/fneur.2020.00957
Chiu D, Peterson L, Elkind MSV, Rosand J, Gerber LM, Silverstein MD. Comparison of outcomes after intracerebral hemorrhage and ischemic stroke. J Stroke Cerebrovasc Dis 2010; 19: 225-9. https://doi.org/10.1016/j.jstrokecerebrovasdis.2009.06.002
Zhang Y, Wang Y, Ji R, Wang A, Wang Y, Yang Z, et al. In-hospital complications affect short-term and long-term mortality in ICH: A prospective cohort study. Stroke Vasc Neurol 2021; 6: 201-6. https://doi.org/10.1136/svn-2020-000386
Tanne D, Kasner SE, Demchuk AM, Koren-Morag N, Hanson S, Grond M, et al. Markers of increased risk of intracerebral hemorrhage after intravenous recombinant tissue plasminogen activator therapy for acute ischemic stroke in clinical practice: The multicenter rt-PA acute stroke survey. Circulation 2002; 105: 1679-85. https://doi.org/10.1161/01.CIR.0000012747.53592.6A
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke a guideline for healthcare professionals from the American Heart Association/American Stroke. Stroke 2019; 50: e344-418. https://doi.org/10.1161/STR.0000000000000211
Alberti KGMM, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus. Provisional report of a WHO consultation. Diabet Med 1998; 15: 539-53. https://doi.org/10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S
Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, et al. Definition and classification of chronic kidney disease: A position statement from Kidney Disease: Improving Global Outcomes (KDIGO)z. Kidney Int 2005; 67: 2089-100. https://doi.org/10.1111/j.1523-1755.2005.00365.x
Mechanic OJ, Gavin M, Grossman SA. Acute Myocardial Infarction. [Updated 2023 3 September]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK459269
Malik A, Brito D, Vaqar S, Chhabra L. Congestive Heart Failure. [Updated 2023 5 November]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430873
Fiorelli M, Bastianello S, von Kummer R, del Zoppo GJ, Larrue V, Lesaffre E, et al. Hemorrhagic transformation within 36 hours of a cerebral infarct. Stroke 1999; 30: 2280-4. https://doi.org/10.1161/01.STR.30.11.2280
Hacke W, Kaste M, Fieschi C, Von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Lancet 1998; 352: 1245-51. https://doi.org/10.1016/S0140-6736(98)08020-9
Bluhmki E, Chamorro Á, Dávalos A, Machnig T, Sauce C, Wahlgren N, et al. Stroke treatment with alteplase given 3·0-4·5 h after onset of acute ischaemic stroke (ECASS III): additional outcomes and subgroup analysis of a randomised controlled trial. Lancet Neurol 2009; 8: 1095-102. https://doi.org/10.1016/S1474-4422(09)70264-9
Dharmasaroja PA, Muengtaweepongsa S, Dharmasaroja P. Intravenous thrombolysis in Thai patients with acute ischemic stroke: Role of aging. J Stroke Cerebrovasc Dis 2013; 22: 227-31. https://doi.org/10.1016/j.jstrokecerebrovasdis.2011.08.001
Wattanawong R, Ratanakorn D, Keandoungchun J. Comparison of predictive scores for symptomatic intracerebral hemorrhage after intravenous thrombolysis in Thai stroke patients. J Thai Stroke Soc 2015; 14: 175.
National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995; 333: 1581-7. https://doi.org/10.1056/NEJM199512143332401
Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al; ECASS Investigators. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008; 359: 1317-29. https://doi.org/10.1056/NEJMoa0804656
Fisher M, Ringleb PA, Schellinger PD, Schranz C, Hacke W. Thrombolytic therapy within 3 to 6 hours after onset of ischemic stroke: Useful or harmful? Stroke 2002; 33: 21437-41. https://doi.org/10.1161/01.STR.0000015555.21285.DB
Derex L, Nighoghossian N. Intracerebral haemorrhage after thrombolysis for acute ischaemic stroke: an update. J Neurol Neurosurg Psychiatry 2008; 79: 1093-9. https://doi.org/10.1136/jnnp.2007.133371
Rodríguez-Yáñez M, Castellanos M, Blanco M, García MM, Nombela F, Serena J, et al. New-onset hypertension and inflammatory response/poor outcome in acute ischemic stroke. Neurology 2006; 67: 1973-8. https://doi.org/10.1212/01.wnl.0000247064.53130.91
Yaghi S, Willey JZ, Cucchiara B, Goldstein JN, Gonzales NR, Khatri P, et al. Treatment and outcome of hemorrhagic transformation after intravenous alteplase in acute ischemic stroke a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2017; 48: e343-61. https://doi.org/10.1161/STR.0000000000000152
Park C, Charalambous LT, Yang Z, Adil SM, Hodges SE, Lee HJ, et al. Inpatient mortality and healthcare resource utilization of nontraumatic intracerebral hemorrhage complications in the US. J Neurosurg 2021; 135: 1081-90. https://doi.org/10.3171/2020.8.JNS201839
LaForce FM. Hospital-acquired gram-negative rod pneumonias: an overview. Am J Med 1981; 70: 664-9. 27. Alsumrain M, Melillo N, Debari VA, Kirmani J, Moussavi M, Doraiswamy V, et al. Predictors and outcomes of pneumonia in patients with spontaneous intracerebral hemorrhage. J Intensive Care Me. 2013; 28: 118-23. https://doi.org/10.1177/0885066612437512
Molina CA, Alvarez-Sabín J, Montaner J, Abilleira S, Arenillas JF, Coscojuela P, et al. Thrombolysis-related hemorrhagic infarction: A marker of early reperfusion, reduced infarct size, and improved outcome in patients with proximal middle cerebral artery occlusion. Stroke 2002; 33: 1551-6. https://doi.org/10.1161/01.STR.0000016323.13456.E5
Verin E, Clavé P, Bonsignore MR, Marie JP, Bertolus C, Similowski T, et al. Oropharyngeal dysphagia: When swallowing disorders meet respiratory diseases. Eur Respir J 2017; 49: 1602530. https://doi.org/10.1183/13993003.02530-2016
Yu S, Arima H, Heeley E, Delcourt C, Krause M, Peng B, et al. White blood cell count and clinical outcomes after intracerebral hemorrhage: The INTERACT2 trial. J Neurol Sci 2016; 361: 112-6. https://doi.org/10.1016/j.jns.2015.12.033
Saand AR, Yu F, Chen J, Chou SHY. Systemic inflammation in hemorrhagic strokes - A novel neurological sign and therapeutic target? J Cereb Blood Flow Metab 2019; 39: 959-88. https://doi.org/10.1177/0271678X19841443
Lambertsen KL, Biber K, Finsen B. Inflammatory cytokines in experimental and human stroke. J Cereb Blood Flow Metab 2012; 32: 1677-98. https://doi.org/10.1038/jcbfm.2012.88
Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. Lancet 2000; 355: 1670-4. https://doi.org/10.1016/S0140-6736(00)02237-6
Dzialowski I, Hill MD, Coutts SB, Demchuk AM, Kent DM, Wunderlich O, et al. Extent of early ischemic changes on computed tomography (CT) before thrombolysis: Prognostic value of the Alberta Stroke Program early CT score in ECASS II. Stroke 2006; 37: 973-8. https://doi.org/10.1161/01.STR.0000206215.62441.56
Na DG, Sohn CH, Kim EY. Imaging-based management of acute ischemic stroke patients: Current neuroradiological perspectives. Korean J Radiol 2015; 16: 372-90. https://doi.org/10.3348/kjr.2015.16.2.372
Chen CJ, Brown WM, Moomaw CJ, Langefeld CD, Osborne J, Worrall BB, et al. Alcohol use and risk of intracerebral hemorrhage. Neurology 2017; 88: 2043-51. https://doi.org/10.1212/WNL.0000000000003952
Downloads
Additional Files
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.