IMPROVING QUALITY OF LIFE IN LOCALLY ADVANCED OR ADVANCED HEAD AND NECK CANCER WITH CURCUMIN ADD-ON TO STANDARD NUTRITION SUPPORT: A SECONDARY ANALYSIS OF THE CURCHEXIA STUDY
DOI:
https://doi.org/10.55374/jseamed.v9.234Keywords:
curcumin, head and neck cancer, HNSCC, cancer cachexia, quality of life, QoL, nutritional support, pharmaconutrientAbstract
Background: Patients with head and neck cancer often suffer from cancer anorexia and cachexia syndrome (CAS), which severely impacts their quality of life (QoL). The primary CurChexia study showed that curcumin improved muscle mass. Objectives: This pre-planned secondary analysis evaluated the effect of curcumin add-on therapy on the QoL of these patients.
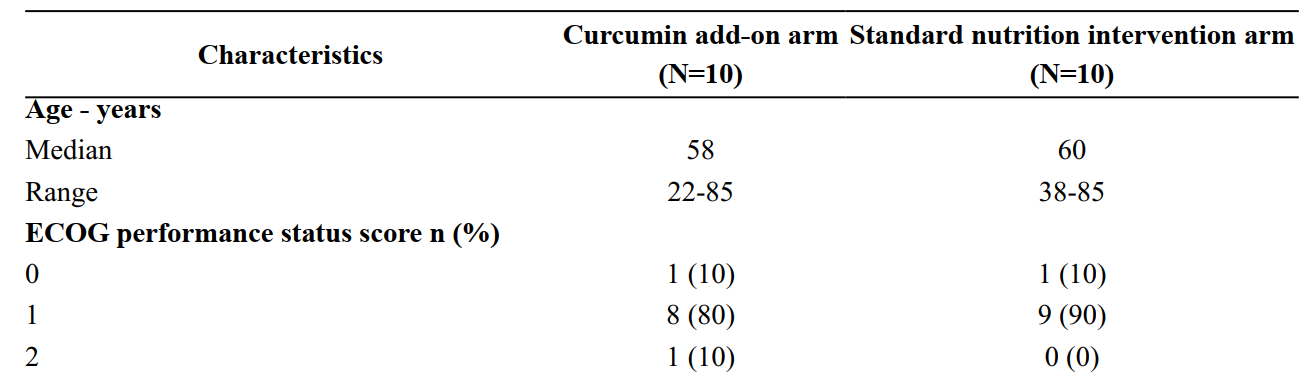
Methods: In this secondary analysis of a randomized, placebo-controlled trial, twenty patients with locally advanced or advanced head and neck cancer undergoing treatment and diagnosed with CAS were randomized to receive either 4,000 mg of curcumin daily or a placebo, in addition to standard nutritional support for eight weeks. QoL was assessed at baseline, week 4, and week 8 using the EORTC QLQ-C30 questionnaire. A linear mixed-effects model was used to analyze changes in QoL scores over time between the two groups. A retrospective power calculation was conducted for key QoL domains.
Results: The curcumin add-on group showed statistically significant improvements compared to the control group in physical functioning (p = 0.001), emotional functioning (p = 0.023), appetite loss (p = 0.001), and pain (p = 0.033). No significant differences were observed in global health status or other functional and symptom scales. The study was adequately powered (>80%) to detect the observed significant differences, but was underpowered for non-significant outcomes like global health status.
Conclusion: In patients with locally advanced or advanced head and neck cancer experiencing cancer anorexia-cachexia syndrome (CAS) during treatment, the addition of a daily 4,000 mg dose of curcumin to standard nutritional intervention significantly improves quality of life and body composition. These findings suggest that curcumin may serve as an effective pharmaconutrient, providing both clinical benefits and supportive care.
Downloads
Metrics
References
Argiles JM, Busquets S, Stemmler B, LopezSoriano FJ. Cancer cachexia: understanding the molecular basis. Nat Rev Cancer 2014; 14: 754–62. DOI: https://doi.org/10.1038/nrc3829
Argiles JM, Lopez-Soriano FJ. The ubiquitin-dependent proteolytic pathway in skeletal muscle: its role in pathological states. Trends Pharmacol Sci 1996; 17: 223–6. DOI: https://doi.org/10.1016/0165-6147(96)10021-3
van Royen M, Carbo N, Busquets S, Alvarez B, Quinn LS, Lopez-Soriano FJ, et al. DNA fragmentation occurs in skeletal muscle during tumor growth: A link with cancer cachexia? Biochem Biophys Res Commun 2000; 270: 533–7. DOI: https://doi.org/10.1006/bbrc.2000.2462
Argiles JM, Busquets S, Toledo M, LopezSoriano FJ. The role of cytokines in cancer cachexia. Curr Opin Support Palliat Care 2009; 3: 263–8. DOI: https://doi.org/10.1097/SPC.0b013e3283311d09
Siddiqui RA, Hassan S, Harvey KA, Rasool T, Das T, Mukerji P, et al. Attenuation of proteolysis and muscle wasting by curcumin c3 complex in MAC16 colon tumour-bearing mice. Br J Nut 2009; 102: 967–75. DOI: https://doi.org/10.1017/S0007114509345250
Gil da Costa RM, Aragao S, Moutinho M, Alvarado A, Carmo D, Casaca F, et al. HPV16 induces a wasting syndrome in transgenic mice: Amelioration by dietary polyphenols via NF-kappaB inhibition. Life Sci 2017; 169: 11–9. DOI: https://doi.org/10.1016/j.lfs.2016.10.031
Gupta SC, Kim JH, Kannappan R, Reuter S, Dougherty PM, Aggarwal BB. Role of nuclear factor kappaB-mediated inflammatory pathways in cancer-related symptoms and their regulation by nutritional agents. Exp Biol Med (Maywood) 2011; 236: 658–71. DOI: https://doi.org/10.1258/ebm.2011.011028
Prasongsook N, Sitalarom K, Saichaemchan S, Peechatanan K, Chaiworramukkul A. A double-blind, placebo-controlled randomized phase II study: Evaluating the effect of curcumin for treatment of cancer anorexiacachexia syndrome in solid cancer patients. J Clin Oncol 2019; 37(15_suppl): e23151–e. DOI: https://doi.org/10.1200/JCO.2019.37.15_suppl.e23151
Chainani-Wu N. Safety and anti-inflammatory activity of curcumin: a component of tumeric (Curcuma longa). J Altern Complement Med 2003; 9: 161–8. DOI: https://doi.org/10.1089/107555303321223035
Thambamroong T, Seetalarom K, Saichaemchan S, Pumsutas Y, Prasongsook N. Efficacy of curcumin on treating cancer anorexia-cachexia syndrome in locally or advanced head and neck cancer: A double-blind, placebo-controlled randomised phase IIa trial (CurChexia). J Nutr Metab 2022; 2022: 5425619. DOI: https://doi.org/10.1155/2022/5425619
Silpakit C, Sirilerttrakul S, Jirajarus M, Sirisinha T, Sirachainan E, Ratanatharathorn V. The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C30): validation study of the Thai version. Qual Life Res 2006; 15: 167–72. DOI: https://doi.org/10.1007/s11136-005-0449-7
Fayers P, Aaronson NK, Bjordal K, Sullivan M. EORTC QLQ–C30 Scoring Manual. Brussels: European Organisation for Research and Treatment of Cancer; 1995.
Osoba D, Rodrigues G, Myles J, Zee B, Pater J. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 1998; 16: 139–44. DOI: https://doi.org/10.1200/JCO.1998.16.1.139
Osoba D, Bezjak A, Brundage M, Zee B, Tu D, Pater J. Analysis and interpretation of health-related quality-of-life data from clinical trials: basic approach of The National Cancer Institute of Canada Clinical Trials Group. Eur J Cancer 2005; 41: 280–7. DOI: https://doi.org/10.1016/j.ejca.2004.10.017
Tseng CH, Elashoff R, Li N, Li G. Longitudinal data analysis with non-ignorable missing data. Stat Methods Med Res 2016; 25: 205– 20. DOI: https://doi.org/10.1177/0962280212448721
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr 2017; 36: 11–48. DOI: https://doi.org/10.1016/j.clnu.2016.07.015
Muscaritoli M, Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, et al. ESPEN practical guideline: Clinical Nutrition in Cancer. Clin Nutr 2021; 40: 2898–913. DOI: https://doi.org/10.1016/j.clnu.2021.02.005
Saeteaw M, Sanguanboonyaphong P, Yoodee J, Craft K, Sawangjit R, Ngamphaiboon N, et al. Efficacy and safety of pharmacological cachexia interventions: systematic review and network meta-analysis. BMJ Support Palliat Care 2021; 11: 75–85. DOI: https://doi.org/10.1136/bmjspcare-2020-002601
Cai D, Frantz JD, Tawa NE, Jr., Melendez PA, Oh BC, Lidov HG, et al. IKKbeta/ NF-kappaB activation causes severe muscle wasting in mice. Cell 2004; 119: 285–98. DOI: https://doi.org/10.1016/j.cell.2004.09.027
Tisdale MJ. Catabolic mediators of cancer cachexia. Curr Opin Support Palliat Care 2008; 2: 256–61. DOI: https://doi.org/10.1097/SPC.0b013e328319d7fa
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Journal of Southeast Asian Medical Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.