ASSOCIATION BETWEEN CORE MUSCLES ACTIVATION AND THE 400-METER OVERGROUND SPRINTING VELOCITY IN WHEELCHAIR RACERS
DOI:
https://doi.org/10.55374/jseamed.v2i2.12Keywords:
Athlete athletics, Disabilities, Paraplegia, Sports, PropulsionAbstract
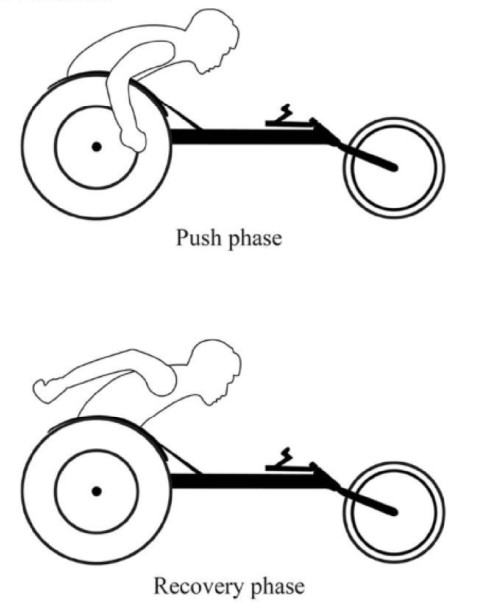
Objective: To measure the activity of the core muscles and the middle trapezius in T54 class wheelchair racers during full-effort over ground sprinting and to determine its association with propulsion velocity. Material and Method: Eightmale international wheelchair racershaving normal upper limband partial to normaltrunk function(T54 class athletes) propelled their racing wheelchairs on 400-m competition trackwith maximal effort. Electromyography(EMG)of the rectus abdominis (RA), iliocostalis lumborum (IL), longissimus thoracis (LT) and middle trapezius (MT) were recorded at each 100-m reach using a wireless surface EMG recorder. Percentage of maximal voluntary contraction (%MVC)was measuredand correlated with propulsion velocity. Results:Median %MVC of RA, IL, LT and MT were 54.2, 43.9, 30.6 and 35.6% respectively. Positive associationto propulsion velocity was found in RA (p = 0.04, r = 0.73). Negative association to propulsion velocity was also found in MT (p = 0.03, r = -0.77). Conclusion: Abdominal function wasactivated most andassociated with propulsion velocity in male T54 class wheelchair racers. In addition, optimizing scapularretraction may benefit propulsionvelocity.
Downloads
Metrics
References
Moss AD, Fowler NE, Goosey-Tolfrey VL. The intra-push velocity profile of the over-ground racing wheelchair sprint start. J Biomech2005;38:15-22. DOI: https://doi.org/10.1016/j.jbiomech.2004.03.022
Vanlandewijck Y, Theisen D, Daly D. Wheelchair propulsion biomechanics: implications for wheelchair sports. Sports med 2001;31:339-67. DOI: https://doi.org/10.2165/00007256-200131050-00005
Kumerddee W, Tongsiri N. Corelation between anaerobic fitness and starting velocity in Thai national team wheelchair racers. J Thai Rehabil Med 2010:20:68-72.
Chow JW, Levy CE. Wheelchair propulsion biomechanics and wheelers' quality of life: an exploratory review. Disabil Rehabil Assist Technol 2011;6:365-77. DOI: https://doi.org/10.3109/17483107.2010.525290
van der Woude LH, Bakker WH, Elkhuizen JW, Veeger HEJ, Gwinn T. Propulsion technique and anaerobic work capacity in elite wheelchair athletes: cross-sectional analysis. Am J Phys Med Rehabil1998;77: 222-34. DOI: https://doi.org/10.1097/00002060-199805000-00007
Wang YT, Deutsch H, Morse M, Hedrick B, Millikan T. Three-dimensional kinematics of wheelchair propulsion across racing speeds. Adapt Phys Act Q 1995;12:78-89. DOI: https://doi.org/10.1123/apaq.12.1.78
Limrungreungrat W. and Wang YT. Three-dimensional pushrim force during different racing wheelchair propulsion speeds. In: Routledge handbook of ergonomics in sport and exercise. 1 edn. New York: Roudledge, 2014. pp. 549-56.
Chow JW, Millikan TA, Carlton LG, Morse MI, Chae WS. Biomechanical comparison of two racing wheelchair propulsion techniques. Med Sci Sports Exerc 2001;33:476-84. DOI: https://doi.org/10.1097/00005768-200103000-00022
Guo LY, Su FC, An KN. Effect of handrim diameter on manual wheelchair propulsion: mechanical energy and power flow analysis. Clin biomech 2006;21:107-15. DOI: https://doi.org/10.1016/j.clinbiomech.2005.08.015
Willardson JM. Core stability training: applications to sports conditioning programs. J Strength Cond Res 2007;21:979-85. DOI: https://doi.org/10.1519/00124278-200708000-00054
Mautner KR, Huggins MJ. The young adult spine in sports. Clin Sports Med 2012;31:453-72. DOI: https://doi.org/10.1016/j.csm.2012.03.007
Shinkle J, Nesser TW, Demchak TJ, McMannus DM. Effect of core strength on the measure of power in the extremities. J Strength Cond Res 2012;26:373-80. DOI: https://doi.org/10.1519/JSC.0b013e31822600e5
Hill J, Leiszler M. Review and role of plyometrics and core rehabilitation in competitive sport. Curr sports med rep 2011;10:345-51. DOI: https://doi.org/10.1249/JSR.0b013e31823b3b94
Bliss LS, Teeple P. Core stability: the centerpiece of any training program. Curr sports med rep 2005;4:179-83. DOI: https://doi.org/10.1097/01.CSMR.0000306203.26444.4e
Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sports med 2006;36:189-98. DOI: https://doi.org/10.2165/00007256-200636030-00001
Hibbs AE, Thompson KG, French D, Wrigley A, Spears I. Optimizing performance by improving core stability and core strength. Sports med 2008;38:995-1008. DOI: https://doi.org/10.2165/00007256-200838120-00004
Sato K, Mokha M. Does core strength training influence running kinetics, lower-extremity stability, and 5000-M performance in runners? J Strength Cond Res 2009;23:133-40. DOI: https://doi.org/10.1519/JSC.0b013e31818eb0c5
Saeterbakken AH, van den Tillaar R, Seiler S. Effect of core stability training on throwing velocity in female handball players. J Strength Cond Res 2011;25:712-18. DOI: https://doi.org/10.1519/JSC.0b013e3181cc227e
Borghuis AJ, Lemmink KA, Hof AL. Core muscle response times and postural reactions in soccer players and nonplayers. Med Sci Sports Exerc 2011;43:108-14. DOI: https://doi.org/10.1249/MSS.0b013e3181e93492
Guo LY, Su FC, Wu HW, An KN. Mechanical energy and power flow of the upper extremity in manual wheelchair propulsion. Clin biomech 2003;18:106-14. DOI: https://doi.org/10.1016/S0268-0033(02)00177-8
Kibler B. Biomechanical analysis of the shoulder during tennis activities. In: Clinics in sports medicine, racquet sports. Richard C. Lehman, eds. Philadelphia: W.B. Saunders company, 1995. pp. 79-85. DOI: https://doi.org/10.1016/S0278-5919(20)30259-3
Kaczmarek P, Lubiatowski P, Cisowski P, Grygorowicz M, ?epski M, D?ugosz J, Ogrodowicz P, Dudzi?ski W, Nowak M, Romanowski L. Shoulder problems in overhead sports. Part I - biomechanics of throwing. Pol Orthop Traumatol. 2014;15:50-58.
Paine R, Voight ML. The role of the scapula. Int J Sports Phys Ther. 2013;8:617-29.
Mulroy SJ, Gronley JK, Newsam CJ, Perry J. Electromyographic activity of shoulder muscles during wheelchair propulsion by paraplegic persons. Arch Phys Med Rehabil 1996;77:187-93. DOI: https://doi.org/10.1016/S0003-9993(96)90166-5
International Paralympic Committee. IPC Athletics Classification. Handbook of IPC athletics classification workshop, 2006. pp. 10-11.
Konrad P. Signal processing-amplitude normalization, The ABC of EMG-A practical introduction to kinesiological electromyography. Scottsdale: Noraxon U.S.A., 2006. pp. 15.
Criswell E. Electrode placements. In: Cram's introduction to surface electromyography. 2 edn. Sudbury, Massachusetts: Jones and Barlett Publishers, 2011. pp. 257-384.
Rankin JW, Richter WM, Neptune RR. Individual muscle contributions to push and recovery subtasks during wheelchair propulsion. J Biomech 2011;44:1246-52. DOI: https://doi.org/10.1016/j.jbiomech.2011.02.073
Tweedy S. Research report, IPC athletics classification project for physical impairments: final report – stage 1. University of Queensland, 2009. pp. 37.
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Southeast Asian Medical Research will hold the copyright to all published articles. The publisher's production department handles copyright forms once a manuscript is accepted and scheduled for publication.